Surgery is a core component of health. It is a cost-effective intervention1 which is important for global health.2 However, to fully realize the health benefits of surgery, it needs to be safe. In the African continent—with a population of 1.2 billion people—it is estimated that approximately 95% do not have access to safe and affordable surgery. The Lancet Commission on Global Surgery has established six indicators to indicate the success of providing access to safe and affordable surgery.3 Four of them are included in the World Bank’s World Development Indicators (WDI) database. The perioperative mortality rate (POMR)—the number of in-hospital deaths from any cause in patients who have undergone a procedure done in an operating theatre, divided by the total number of procedures—is one of the indicators the success in achieving safe surgery, yet it is not included in the WDI as the data is sparse, including the one from Africa. The recent publication of the African Surgical Outcomes Study (ASOS) has cast an important light on the POMR in Africa.4
ASOS has shown that for patients in Africa fortunate enough to access surgical care, the patient outcomes following surgery are relatively poor. ASOS demonstrated that African surgical patients were twice as likely to die following surgery when compared to the global average, despite a similar complication rate to the global average (Table 1). This is despite the fact that surgical patients in Africa are relatively healthy when compared with similar international surgical patient cohorts,5 and one would thus expect them to do well postoperatively. Therefore, if the data from ASOS had been risk-adjusted for patient comorbidities, it is likely that the mortality following surgery in Africa is more than twice the global average. The results from ASOS are compelling as they provide comprehensive data on surgical outcomes in Africa, from 25 countries, 247 hospitals, and over 11,000 patients.
Table 1. Mortality, complications and ‘failure to rescue’ following surgery
| ISOS (elective surgery) |
ASOS (elective surgery) |
ASOS (elective and emergency surgery) |
|
| Mortality | 207/44 814 (0.5%) | 48/4792 (1.0%) | 239/11193 (2.1%) |
| Complications | 7508/44814 (16.8%) | 624/4658 (13.4%) | 1977/10885 (18.2%) |
| Death following complication (failure to rescue) |
207/7508 (2.8%) | 30/620 (4.8%) | 188/1970 (9.5%) |
Identifying the possible causes of postoperative mortality
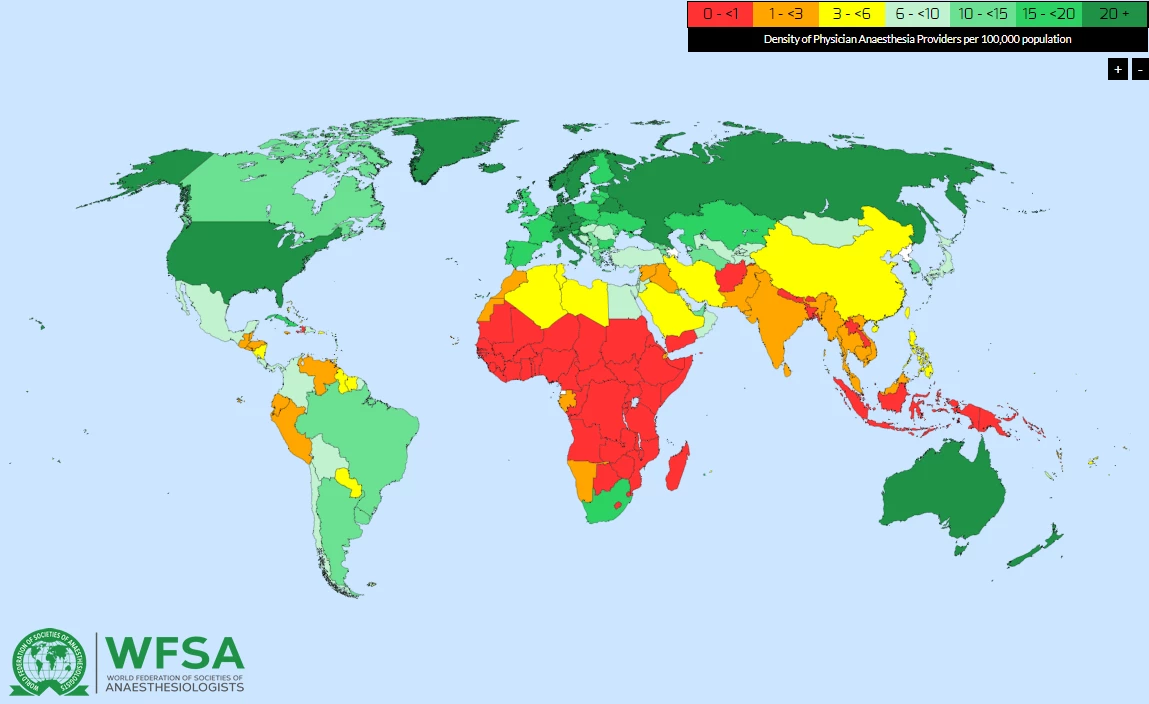
Why are patients twice as likely to die in Africa when compared to the global average? The data from ASOS provide an insight into the paucity of healthcare providers for surgical patients in Africa, and the associated patient outcomes following surgery in Africa. It appears that the increased mortality in Africa is due to two important factors. Firstly, in ASOS the ‘specialist surgical workforce’ (the total number of specialist anaesthetists, surgeons and obstetricians per 100,000 population) was between 20 and 50 times lower than the recommended minimum number needed to provide safe surgical care (20 to 40 per 100 000).2,4,6 More than 80% of Africa has less than one specialist anaesthetist per 100,000 population, which is dramatically illustrated in the interactive workforce map of the World Federation of the Societies of Anaesthesiologists (https://www.wfsahq.org/workforce-map) (Figure 1).7 This is also concerning as it is estimated that at least five physician anaesthesia providers per 100,000 population is necessary to provide safe surgery.
Figure 1. World Federation of the Societies of Anaesthesiologists (WFSA) map of the global physician anaesthetist (specialist) workforce (with permission from the WFSA)
Secondly, the vast majority of the deaths in ASOS occurred in the surgical wards after leaving the operating theatre. It is likely that a major contributor to death following surgery in Africa is a concept known as ‘failure to rescue’. ‘Failure to rescue’ is when patients who develop complications are not identified timeously by the healthcare providers, and consequently do not receive the appropriate care early resulting in excess mortality, which is twice the global average (Table 1). It appears to be a universal problem in Africa, as ‘failure to rescue’ is more common than the global average in every category of postoperative complications (Table 2). In Africa, because there are so few healthcare providers to provide care after surgery, it is likely that patients who develop complications following surgery are often missed in the early course of the complication, and then these complications can progress in severity, and occasionally result in unnecessary deaths following surgery (Figure 2).
Table 2. ‘Failure to rescue’ and mortality following surgical complications in the African Surgical Outcomes Study (ASOS)
| Complications | ISOS (elective surgery) |
ASOS (elective surgery) |
ASOS (elective and emergency surgery) |
| Infectious complications | 104/4032 (2.6%) | 12/354 (3.4%) | 112/1156 (9.7%) |
| Cardiovascular complications | 141/2033 (6.9%) | 15/48 (31.3%) | 110/190 (57.9%) |
| Other complications | 158/5625 (2.8%) | 14/314 (4.5%) | 112/1044 (10.7%) |
| Total complications | 207/7508 (2.8%) | 30/620 (4.8%) | 188/1970 (9.5%) |
Figure 2: The relationship between surgical providers and mortality in Africa
Devising workable solutions
The insights into postoperative mortality provided by ASOS allow us to consider possible interventions that may improve surgical outcomes in Africa. An obvious solution is to increase the number of surgical healthcare providers. Unfortunately, it is unlikely that this will be a solution realised in the short- or even medium-term, as one would need to increase the number of healthcare providers by 20 to 50 times the current workforce.2,4 The country-specific current ‘specialist surgical workforce’ per 100,000 population and the outcomes shown in countries who provided a 'representative' surgical sample in ASOS are shown in Table 3.
Table 3. The country-specific ‘specialist surgical workforce’, and postoperative complications and mortality reported in the African Surgical Outcomes Study (ASOS)4
| Country | Specialist surgical workforce* | % Postoperative complications (95% CI) | % In-hospital mortality (95% CI)† |
| Congo DR | 0.2 | 20.4% (15.9-24.8) | 3.8% (1.7 – 5.9) |
| Gambia | 1.8 | 24.4% (15.1-33.7) | 3.7% (0-7.7) |
| Madagascar | 0.8 | 21.9% (16.0-27.7) | 1.0% (0-2.5) |
| Mali | 1.1 | 22.3% (17.8-26.8) | 3.3% (1.4-5.3) |
| Mauritius | 17.6 | 12.5% (9.3-15.6) | 1.9% (0.6-3.2) |
| Namibia | 6.0 | 18.3% (14.1-22.5) | 3.7% (1.6-5.7) |
| Niger | 0.5 | 38.2% (31.2-45.2) | 1.1% (0-2.6) |
| Nigeria | 1.4 | 17.7% (13.8-21.5) | 2.0% (0.6-3.4) |
| South Africa | 11.5 | 15.4% (14.4-16.3) | 2.4% (2.0-2.8) |
| Uganda | 1.1 | 31.6% (27.9-35.3) | 1.1% (0.3-2.0) |
| Zimbabwe | 1.6 | 11.3% (8.9-13.8) | 1.3% (0.4-2.1) |
*The World Bank ‘Specialist Surgical Workforce’ data ( http://databank.worldbank.org/data/reports.aspx?source=2&series=SH.MED.SAOP.P5)
**ASOS data where World Bank data is absent presented as median [interquartile range]
†The country specific crude mortality rates and complication rates are particularly unstable as ASOS was not powered to accurately determine the country specific mortality and complication rates.
An alternative solution to decrease death following surgery in Africa, may be found in assisting the existing healthcare providers to identify surgical patients who may be at risk of complications following surgery, and providing them with the tools to manage the common postoperative complications. These higher risk surgical patients could be more intensely monitored after surgery, and hopefully get earlier appropriate treatment for their complications before their condition deteriorates further. The African Surgical OutcomeS-2 (ASOS-2) Trial has adopted this approach of increased surveillance of higher risk patients to improving outcomes following surgery in Africa. It is hoped that this trial will provide a simple, pragmatic solution to improving surgical outcomes in Africa. The ASOS-2 Trial will run in 2019.
Finally, the study gives a snapshot of POMR estimates and highlights the need of ongoing data collection of POMR. The ASOS collaborative has created a large network of investigators across Africa, and it is expected to continue to grow with further ASOS projects. This network can provide the infrastructure to support regularly reporting of the POMR in Africa, which is necessary to document our success in providing safer surgery in Africa.
REFERENCES
- Chao TE, Sharma K, Mandigo M, et al. Cost-effectiveness of surgery and its policy implications for global health: a systematic review and analysis. Lancet Glob Health 2014;2(6):e334-45. doi: 10.1016/S2214-109X(14)70213-X [published Online First: 2014/08/12]
- Meara JG, Leather AJ, Hagander L, et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet 2015;386(9993):569-624. doi: 10.1016/S0140-6736(15)60160-X
- Ng-Kamstra J, Raykar N, Meara JG, et al. Measuring surgical systems: a new paradigm for health systems strengthening. The Data Blog. The World Bank: The World Bank, 2016.
- Biccard BM, Madiba TE, Kluyts HL, et al. Perioperative patient outcomes in the African Surgical Outcomes Study: a 7-day prospective observational cohort study. Lancet 2018 doi: 10.1016/s0140-6736(18)30001-1 [published Online First: 2018/01/08]
- Global patient outcomes after elective surgery: prospective cohort study in 27 low-, middle- and high-income countries. Br J Anaesth 2016;117(5):601-09. doi: 10.1093/bja/aew316 [published Online First: 2016/11/02]
- Dare AJ, Onajin-Obembe B, Makasa EM. A snapshot of surgical outcomes and needs in Africa. Lancet 2018 doi: 10.1016/s0140-6736(18)30002-3 [published Online First: 2018/01/08]
- Kempthorne P, Morriss WW, Mellin-Olsen J, et al. The WFSA Global Anesthesia Workforce Survey. Anesth Analg 2017;125(3):981-90. doi: 10.1213/ane.0000000000002258 [published Online First: 2017/07/29]




Join the Conversation