Read the transcript
- 00:00 [Upbeat Music]
- 00:02 [Annual Meetings 2021]
- 00:14 [COMING UP] [ENDING THE PANDEMIC: THE ROAD TO AN INCLUSIVE RECOVERY]
- 00:22 Hello and welcome to Ending the Pandemic,
- 00:26 The Road to an Inclusive Recovery.
- 00:29 I'm Becky Addison live from CNN's Broadcasting Hub
- 00:32 here in Abu Dhabi in the UAE,
- 00:35 [BECKY ANDERSON, CNN PRESENTER] bringing you this special event
- 00:37 alongside the 2021 World Bank-IMF Annual Meetings.
- 00:42 Today, we've reached a critical moment.
- 00:45 We can either take urgent action to end the pandemic
- 00:49 and get the global economy back on track, or
- 00:52 we must reconcile ourselves with the world
- 00:54 where the pandemic will ebb and flow
- 00:56 and where our economies will never reach their true potential.
- 01:01 Here's the deal.
- 01:02 If we want to move beyond this pandemic,
- 01:06 we must make sure at least 40% of all people, in all countries,
- 01:12 are vaccinated by the end of this year.
- 01:16 That is the message from the leaders
- 01:19 I have joining me here today.
- 01:20 They have come together establishing a task force
- 01:24 aimed at doing just that.
- 01:27 I'm delighted to be joined from Washington
- 01:30 by the World Bank President David Malpass,
- 01:34 IMF Chief Kristalina Georgieva,
- 01:39 the WTO Director-General Ngozi Okonjo-Iweala,
- 01:45 and from Geneva, the WHO Director-General
- 01:49 Tedros Adhanom Ghebreyesus.
- 01:54 Choices we make in the coming years will determine
- 01:57 whether developing countries suffer a lost decade
- 02:00 or can usher in rapid growth and economic transformation.
- 02:04 Those are the worlds of the World Bank head, David Malpass.
- 02:08 Bottom line, we can't recover without global cooperation and coordination.
- 02:12 We can't get there without tackling vaccine inequality.
- 02:16 According to the Global Dashboard for Vaccine Equity,
- 02:20 established in part by the WHO as of October 6th,
- 02:24 61% of those living in high income countries
- 02:28 have been jabbed with at least one shot.
- 02:32 That figure drops to less than 4% in low-income countries.
- 02:38 Less than 4%.
- 02:41 Let that sink in.
- 02:44 The goal of the Multilateral Leaders Task Force
- 02:47 is to figure out essentially how to close this gap.
- 02:50 To suggest that there is an alarming shortage of supply
- 02:54 is to, frankly, understate the extent of the problem.
- 02:58 So, David, I'd like to start with you this evening.
- 03:01 What is needed to boost vaccine supply and access
- 03:06 in developing countries?
- 03:07 Let's start there.
- 03:10 [DAVID MALPASS] Thanks, Becky. And you're right.
- 03:12 [DAVID MALPASS, PRESIDENT, WORLD BANK GROUP] 40% is the goal
- 03:14 and that's not being achieved.
- 03:16 What we need to do, and it's particularly apparent in Africa
- 03:20 is to get doses to people that are ready to deliver them.
- 03:23 There is plentiful supply.
- 03:26 The production is going up very rapidly
- 03:29 in the advanced economies.
- 03:31 But there's a gap between the donations
- 03:33 and the actual deliveries of those donated doses
- 03:36 in particular Africa.
- 03:39 What we need to do is get the donators,
- 03:44 the countries that have excess vaccines to state and follow through
- 03:48 in an accountable way with the deliveries,
- 03:52 the dates of the delivery, the type of the vaccine
- 03:55 that's going into the developing countries.
- 03:58 World Bank can help in a number of areas.
- 04:01 We have financing available.
- 04:02 We right now have AVAT, a contract within Africa
- 04:06 that's been successful in getting doses to people
- 04:09 We have today 250,000 doses under contract
- 04:14 that will be delivered.
- 04:15 So we're trying to have early delivery dates
- 04:18 for the donations that have been committed
- 04:21 by the advanced economies.
- 04:23 We need to know what type of vaccine is
- 04:27 and where it's going to be delivered
- 04:29 so we can work on the hesitancy problem.
- 04:32 [BECKY ANDERSON] Right. Okay.
- 04:33 Tedros, you and I have been talking
- 04:36 vaccine inequality for over twelve months.
- 04:38 Progress, with respect to all of you, has been painfully slow.
- 04:44 I know, you know that.
- 04:46 Firstly, are these donations enough, sir?
- 04:54 [TEDROS ADHANOM GHEBREYESUS] Yeah. Thank you, Becky.
- 04:56 The donations are not enough.
- 04:58 And to be honest, as you said, very slow.
- 05:01 [DR. TEDROS ADHANOM GHEBREYESUS, DIRECTOR-GENERAL, WHO] Plus,
- 05:04 it's very disappointing that it's taking so long
- 05:08 for the world to really commit.
- 05:11 Epidemiologically, it's wrong
- 05:13 because we cannot end this pandemic.
- 05:15 Economically, it's wrong because the economy globally is not recovering
- 05:21 and it is also morally wrong.
- 05:26 There should be a political commitment to address this problem.
- 05:30 As you have rightly said, if you take low-income countries,
- 05:33 it's only 4%, and if you take it in another way
- 05:37 70% of the deliveries are done just to 10 countries,
- 05:42 That's completely unfair.
- 05:47 This will not end the pandemic.
- 05:49 It's in the interest of all countries
- 05:52 rich, poor or middle-income to end this pandemic.
- 05:57 And that's why, together with my colleagues in the task force,
- 06:01 we are saying there is a 40% by the end of this year target,
- 06:06 and 70% by the mid of next year.
- 06:09 We have to, especially when G20 countries should own those targets
- 06:14 and make it happen
- 06:15 because more than 80% of the economy belongs to them.
- 06:20 The bulk of the production capacity also belongs to them.
- 06:24 If there is political commitment and they want to do it, they can do it.
- 06:28 So that's what we're asking.
- 06:30 [BECKY ANDERSON] That's a big question, though, isn't it?
- 06:32 That's the big question.
- 06:33 Is the political commitment on standby?
- 06:35 I just want to bring other two gets in tonight.
- 06:38 Let's be quite clear about this.
- 06:40 Ngozi, let me start with you.
- 06:42 Just how realistic are these targets at this point?
- 06:46 We are talking at least 40% of people in every country vaccinated
- 06:50 by the end of 2021 and at least 60% by mid 2022.
- 06:56 We are way away from those levels at this point.
- 07:02 [NGOZI OKONJO-IWEALA] Well, thank you very much, Becky.
- 07:05 I think that with these targets,
- 07:07 we are well aware you can see the numbers
- 07:10 [NGOZI OKONJO-IWEALA, DIRECTOR-GENERAL, WTO] that you talked about
- 07:12 4% in low-income countries, 60% in rich countries.
- 07:19 But if you can see the progress that can be made in countries
- 07:23 when they have access to these vaccines
- 07:25 and where the ability to distribute them
- 07:28 and get them into arms there.
- 07:31 So I think if we decide as a community
- 07:35 that we can do this, we will do it.
- 07:37 We are very far away from where we need to be.
- 07:40 But we need to ramp up now
- 07:42 because as Tedros said, it's just not acceptable
- 07:45 that we have this gap.
- 07:47 So let's get the vaccines delivered quickly.
- 07:50 We have countries waiting to put these vaccines into arms.
- 07:55 Let's get them delivered and we may be able
- 07:57 to achieve this target.
- 07:59 This might be ambitious, given where we are now.
- 08:01 But it's not impossible.
- 08:03 [BECKY ANDERSON] Kristalina standby because I do want to get
- 08:06 your perspective on this.
- 08:08 The cold, hard fact, according to Amnesty International,
- 08:13 out of the nearly 6 billion COVID-19 doses delivered worldwide,
- 08:18 a poultry 0.3% have gone to low-income countries.
- 08:23 And at this point I just want to draw on some CNN reporting
- 08:28 to underscore the challenge here.
- 08:30 Let's look at Africa, for example, standby.
- 08:42 [JOHANNESBURG] [SOUTH AFRICA]
- 08:43 [Dave McKenzie] I'm Dave McKenzie in Johannesburg.
- 08:44 If you look around me, life seems to be getting back to normal.
- 08:48 But this country, in this region,
- 08:50 has suffered through a devastating COVID-19 pandemic.
- 08:53 The big issue now, to avoid future waves,
- 08:56 is of course, vaccines.
- 08:58 Vaccine nationalism and vaccine hoarding
- 09:01 has really hit the efforts for an equitable access
- 09:04 across the world, particularly in Africa,
- 09:07 for COVID-19 vaccines.
- 09:08 In the African continent,
- 09:09 there are far less than 10% of people
- 09:12 who've received their full complement of COVID-19 vaccines,
- 09:17 Even as rich countries are giving booster shots
- 09:20 to the most vulnerable.
- 09:22 Now, the issue is,
- 09:23 as manufacturers ramp up vaccination production,
- 09:28 can the money and the resources be made available
- 09:30 to get vaccines optimations on the African continent,
- 09:34 or can there be a deal made
- 09:36 on dropping intellectual property of those vaccines?
- 09:40 All I can say is
- 09:41 through all my reporting on this issue
- 09:43 is the talk of solidarity has largely been talk.
- 09:48 Now it's time for action.
- 09:50 [BECKY ANDERSON] Kristalina, get the money and resources
- 09:52 to where they matter most is David's appeal.
- 09:56 What is being done to address finance and trade barriers
- 10:01 to ensure that vulnerable populations get these life saving tools?
- 10:08 [KRISTALINA GEORGIEVA] Thank you very much for bringing us together, Becky.
- 10:11 What we have seen is
- 10:13 [KRISTALINA GEORGIEVA, MANAGING DIRECTOR, IMF]
- 10:14 much more awareness
- 10:16 of the economic significance of overcoming
- 10:20 this great vaccination divide
- 10:24 and that awareness is slowly translating into
- 10:29 more willingness to act.
- 10:31 So, what do we know?
- 10:34 We know that the world economy is recovering,
- 10:37 that risks are going up
- 10:41 and the divergence in economic fortunes is expanding.
- 10:47 Why would that matters to advanced economies, to rich countries?
- 10:52 Because if the world continues to be slow to recover,
- 10:59 held back a lot by access to vaccines
- 11:03 by limited fiscal space,
- 11:05 that not only causes supply disruptions,
- 11:09 and the supply disruptions are one of the factors
- 11:13 pushing prices up.
- 11:16 But it also creates space for new variants of COVID
- 11:24 to flourish and run around the world.
- 11:26 We have done very careful analysis
- 11:30 that says that for $50 billion dollars,
- 11:35 we can achieve the target of vaccinating 40%
- 11:41 by the end of this year.
- 11:44 70%, actually Tedros lifted up to 70% target by mid 2022.
- 11:53 Of this 50 billion,
- 11:55 we now see close to two thirds being made available.
- 12:02 But we still have a gap to feel.
- 12:06 What are we doing?
- 12:08 I want to praise the World Bank for stepping up.
- 12:12 They are now willing and able to secure 20 billion in financing.
- 12:18 We, the IMF, have provided the largest in our history allocation
- 12:24 of the so called special drawing rights to
- 12:28 reserve assets of the IMF that gives countries fiscal space.
- 12:33 Where are the bottlenecks?
- 12:37 I do strongly believe there are two.
- 12:40 One, it is timely, allocation of vaccines
- 12:46 to developing countries.
- 12:48 If a rich country doesn't need the vaccines in November,
- 12:52 they can receive them in February.
- 12:58 Move the delivery in November to the developing quote.
- 13:03 And secondly, and this is where
- 13:06 it is so important we work together,
- 13:10 getting a vail of vaccine to turn into a shot in the arm.
- 13:16 And in many poor countries,
- 13:18 it is this getting the vaccine from the town where it is stored
- 13:25 to the child or the woman or the man in a village up in the mountains
- 13:31 that is the toughest part of this delivery.
- 13:35 I want to answer your question honestly,
- 13:38 can we get to 40% everywhere?
- 13:40 This is going to be tough.
- 13:42 But can we get much closer to 40% everywhere?
- 13:47 And at more than 40% in many countries?
- 13:51 Yes, the vaccines are produced.
- 13:54 We have to make sure they get
- 13:56 where they would make a difference.
- 13:58 [BECKY ANDERSON] Would a decision by the developed world
- 14:03 to advise booster shots to its populations
- 14:10 prevent you as they task force from achieving your goal?
- 14:15 David.
- 14:16 [DAVID MALPASS] I don't think that's the key issue.
- 14:19 The production is going up so rapidly.
- 14:21 There may be enough to do boosters
- 14:23 and to reach targets in 2022.
- 14:28 The key thing that I would emphasize is
- 14:30 for finance ministers in countries and their health ministers
- 14:34 to seek contracts, to try to get delivery dates that are early
- 14:38 and to ask for them and to request them
- 14:41 and then for the advanced economies
- 14:44 to go along with that to help get the delivery dates.
- 14:48 I was in Sudan.
- 14:50 Well, let me mention two things.
- 14:52 J&J doses are particularly valuable in Africa.
- 14:55 Europe has committed to shipping J&J doses to Africa.
- 15:00 Complete that so the people can have those doses.
- 15:04 I was in Khartoum and then Amman last week.
- 15:07 They're vaccinating people day by day.
- 15:11 The hesitancy is going down as once people have vaccines
- 15:15 and if they have the syringes and the needles
- 15:18 that can be brought in with the shipments of the doses,
- 15:23 then the people are being vaccinated so that part of the system is working.
- 15:28 But we need more clear delivery dates from the various sources.
- 15:32 World bank has 61 countries that have programs with us
- 15:36 and we can expand that into 100 countries.
- 15:40 If the countries ask for doses
- 15:43 and arrange for getting the contract set up
- 15:46 in accountable way, that's key.
- 15:49 [BECKY ANDERSON] Tedros, I have to get your perspective
- 15:54 at this point on boosters?
- 15:58 [TEDROS ADHANOM GHEBREYESUS] Thank you, Becky.
- 16:00 On Boosters, I would go back to the figures
- 16:04 because the world should understand the inequity the injustice.
- 16:09 As I said earlier, 66.5 billion dollars have already been ministered.
- 16:16 Of this, Africa got only 166 million.
- 16:23 166 million for 1.2 billion people,
- 16:27 and the rest 6.3 billion is for the rest of the world.
- 16:31 Then I can show you in a different way.
- 16:34 For instance, if you take South America, North America,
- 16:36 Europe, Asia, China as a region,
- 16:40 all of them are above 50% at least with a single dose,
- 16:43 while Africa is only 7% single dosed or 4.8%.
- 16:49 So as a region, the focus should be that.
- 16:51 Bringing it back to boosters,
- 16:54 when there is only 166 million delivered in Africa for 1.2 billion,
- 17:01 to start with the booster is really the worst we could do
- 17:07 as a global community.
- 17:10 It's unjust and also unfair
- 17:14 because we will not stop this pandemic
- 17:17 by ignoring the whole continent
- 17:20 and the continent which doesn't have any manufacturing capacity or other means.
- 17:25 The world should come back to its senses.
- 17:27 I don't want to spread it by saying all low-income countries,
- 17:31 the concentration of the problem is in one continent.
- 17:35 Let's take that first. So on.
- 17:36 For boosters, for countries to move into boosters
- 17:40 without even providing single doses in Africa,
- 17:43 it is not right.
- 17:45 It has to be stopped
- 17:46 and countries should respect the moratorium.
- 17:49 Of course there are exceptions.
- 17:51 We can use it in immunocompromised populations.
- 17:55 Immunocompromised.
- 17:57 The rest is immoral, unfair, unjust and it has to stand.
- 18:02 [BECKY ANDERSON] Ngozi and Christine, I must get your perspective on this.
- 18:05 Ngozi, briefly.
- 18:08 [NGOZI OKONJO-IWEALA] Briefly, I think one of the ways
- 18:10 to solve this inequity of access,
- 18:12 which I agree totally with Tedros is unacceptable,
- 18:16 is to decentralize production.
- 18:19 If we are going to continue needing boosters
- 18:22 and things like that,
- 18:23 it's evident that we need to decentralize production
- 18:26 to some of the countries that have no capacity.
- 18:29 On the African continent,
- 18:31 there is 17% of the world population
- 18:33 and 0.2% of the manufacturing capacity.
- 18:36 We cannot continue importing 99% of our vaccines
- 18:41 At the WTO, we've actually been working
- 18:44 with manufacturers of these vaccines
- 18:46 to try and help them with their supply chain problems,
- 18:50 monitoring where they are bottled neck
- 18:52 so that they can be able to increase production,
- 18:55 and at the same time, working with them
- 18:57 to encourage them to set up of manufacturing
- 19:00 in emerging markets in developing countries.
- 19:03 And I think, Becky, that is yielding some fruit.
- 19:06 We've now had an announcement by Pfizer
- 19:09 of investment in South Africa and Aspen.
- 19:12 We've heard of Moderna is just saying that
- 19:16 it's going to set up some production facilities on the continent.
- 19:20 But we need to get the capacity to produce.
- 19:25 [BECKY ANDERSON] The three leading vaccine manufacturers,
- 19:28 BioNTech, Moderna and Pfizer could net $130 billion dollars
- 19:32 by the end of this year.
- 19:33 Ngozi, you're right,
- 19:34 We have seen some progress
- 19:36 in manufacturing plants being set up,
- 19:39 but are these manufacturers prolonging this pandemic
- 19:42 by putting profits before people?
- 19:47 [NGOZI OKONJO-IWEALA] We hear a lot about profits before people,
- 19:52 and obviously, if you look at their numbers,
- 19:54 it is true they're earning far more than they ever have.
- 19:59 So that's why we are working with them to say,
- 20:02 "the perception of this profit before the lives of people
- 20:08 is neither good publicly for you, nor for anyone.
- 20:13 So we're working with them to really try to get
- 20:16 partnerships on the continent,
- 20:19 in Latin America as well, in low-income countries,
- 20:22 so that they can demonstrate that for them
- 20:26 it's not profit, but it's people.
- 20:29 It's coming along.
- 20:30 I think we need the manufacturers
- 20:33 because without them, we're not going to be able
- 20:35 to manufacture vaccines, vaccines are complicated.
- 20:38 You need the technology transfer,
- 20:40 the know-how to be able to do it
- 20:43 along with the issues of intellectual property.
- 20:46 So we cannot alienate them but we have to persuade them
- 20:50 that it's better for them to be public citizens
- 20:53 and put people before profit.
- 20:57 [BECKY ANDERSON] Kristalina, I promised I'll come back to you.
- 20:59 I want to get your perspective on the idea that developing world
- 21:03 will go ahead and provide booster shots
- 21:05 when the developing world is in such dire need.
- 21:09 It has been a year since South Africa and India
- 21:12 first call for the suspension of intellectual property protection
- 21:15 on vaccines and related technologies.
- 21:18 This is something Ngozi has just been alluding to.
- 21:20 The UK, Norway, Switzerland and the EU
- 21:23 are still blocking waiver needed to make that happen.
- 21:28 Do you and do your fellow leaders here today
- 21:32 call on countries to back this proposal,
- 21:35 at least until the fight against the pandemic is over.
- 21:40 [KRISTALINA GEORGIEVA] We at IMF actually researched
- 21:42 the question of production versus availability,
- 21:48 and the answer is
- 21:50 production capacity can deliver doses
- 21:56 for countries that still don't have it and it can deliver boosters.
- 22:02 The problem is to prioritize delivery
- 22:07 for those who do not yet have access to vaccines
- 22:11 and for that purpose, what we are pressing for,
- 22:15 actually all four of us,
- 22:17 is disclosure of contracts,
- 22:21 transparency of who bought what, for what delivery date
- 22:27 and is this a good match of the objective we presented:
- 22:31 Vaccinate at least 40% of the world population
- 22:36 at the end of this year.
- 22:37 I can tell you that in our view,
- 22:40 transparency of contracts and delivery schedules
- 22:45 is going to go a long way to optimize the production capacity.
- 22:51 I want to make two more points
- 22:52 on the question of do we want to see more self-reliance?
- 23:00 The answer is yes.
- 23:02 We are very keen that this crisis turns into an opportunity
- 23:08 for Africa to be more self-reliant.
- 23:12 And in fact, I was very pleased
- 23:15 to learn from Senegal that are going to use
- 23:18 a portion of the special drawing rights
- 23:21 we have allocated to Senegal exactly for this purpose.
- 23:25 Our assessment is that if African countries
- 23:29 take 1 billion of the special drawing rights
- 23:33 to move it towards expanding production,
- 23:36 it can do a lot of good for the future.
- 23:39 My second point is to be clear that yes,
- 23:46 we do need more collaboration on all fronts.
- 23:51 Ngozi is the expert of the trade issue,
- 23:54 so I don't want to jump into her field,
- 23:58 but the simple final point I want to make here, Becky, is that
- 24:04 we are so much in this together, we can get out of it only together.
- 24:09 [BECKY ANDERSON] David, the world--
- 24:10 You make a very good point.
- 24:13 David, the World Bank has deployed over $157 billion dollars
- 24:18 to fight the impact of the pandemic.
- 24:21 This is, as I understand, the largest ever crisis response.
- 24:25 I just want our audience here
- 24:28 to get a sense of what financing instruments
- 24:31 you've used and what have been the results?
- 24:33 What's the learning here?
- 24:37 [DAVID MALPASS] This is a mix around the world
- 24:39 of loans and grants, and it goes to health,
- 24:42 it goes to education,
- 24:44 it goes to governments when they're making positive changes
- 24:48 in their laws that make them more attractive for business,
- 24:51 for setting up vaccine operations.
- 24:54 Part of that 157 billion is the supply of vaccines.
- 24:58 IFC, our private sector arm invests debt and equity
- 25:03 in vaccine manufacturing in Africa,
- 25:05 we're helping expand the Aspen Pharmaceutical in South Africa,
- 25:10 and we're helping research other sites
- 25:14 where vaccine manufacturing can occur.
- 25:16 So there's a range of investments made in development.
- 25:21 from that $157 billion dollars.
- 25:24 And remember, it's a leverage from donors.
- 25:28 Donors put money in and we borrow heavily against it
- 25:32 in capital markets.
- 25:33 It brings in people from around the world together
- 25:37 in sustainable development efforts.
- 25:39 Climate is a core one that's expanding rapidly as well.
- 25:43 [BECKY ANDERSON] Now, I understand that.
- 25:45 Ngozi, I just want to come to you at this point.
- 25:47 The WTO was created, of course, in 1995,
- 25:51 in part to address how trade could be used
- 25:54 to promote sustainable development.
- 25:57 I just wonder, this is a question that I've been asked myself
- 26:02 over the last 19 months,
- 26:04 whether the WTO has actually failed
- 26:08 low-income countries in this instance.
- 26:11 I just wonder what your response to that is.
- 26:14 [NGOZI OKONJO-IWEALA] I would say my response is no,
- 26:17 the WTO has not failed low-income countries in this instance,
- 26:21 this is actually an opportunity, a time
- 26:24 when the WTO and trade have responded very well.
- 26:29 People do not know it but last year,
- 26:33 as the value of trade fell by more than 7%,
- 26:38 the value of medical supplies and products
- 26:41 being treated rose by 16%.
- 26:44 and personal protective equipment by 50%.
- 26:47 What does this mean?
- 26:49 The trade backed by WTO's rules was actually moving goods around
- 26:56 to where they were needed.
- 26:57 Secondly, you mentioned the issue of the TRIPS earlier on.
- 27:02 You talked about the TRIPS waiver and the IP.
- 27:06 Of course, it's a WTO agreement.
- 27:09 More than 100 countries asked our members,
- 27:12 they are asking for a waiver of the intellectual properties rights
- 27:17 so they can have access to this to manufacture vaccines.
- 27:21 We have other members who think that if you do this,
- 27:26 it will get in the way of innovation.
- 27:29 So what are we trying to do?
- 27:31 Actually, there's an emerging consensus from our members now,
- 27:34 after a lot of debate and discussion,
- 27:37 that we need a solution to the IP problem.
- 27:40 People are dying and it's unconscionable.
- 27:43 We should not solve this.
- 27:45 As I said to you, there are discussions going on
- 27:49 for a pragmatic solution and I think we will get it, Becky.
- 27:52 This will allow developing countries
- 27:54 access to know-how technology transfer.
- 27:58 and then, at the same time, in a way that will show
- 28:02 those who have developed these vaccines that they will be protected.
- 28:06 We are not going to disincentivize research--
- 28:09 [BECKY ANDERSON] Ngozi, with respect,
- 28:11 there will be people who will be quite cynical
- 28:15 about what that solution might look like.
- 28:17 So can you just explain what you think it might look like?
- 28:21 [NGOZI OKONJO-IWEALA] This is something being discussed
- 28:25 at the moment by members,
- 28:27 so I cannot say what the ultimate solution will be.
- 28:32 I wanted to say that I'm pretty sure
- 28:34 it will allow better access than we have now,
- 28:37 from some provisions in our TRIPS Agreement
- 28:41 and make it easier for countries to get access.
- 28:44 We have to find the way of bridging this gap.
- 28:47 We all really agree it is not right that people should be dying.
- 28:51 We need to make sure that technology is transferred,
- 28:55 developing countries can manufacture.
- 28:57 I can't put on the table now because they're negotiating
- 29:01 it at this moment.
- 29:02 So I can't tell you the ultimate answer,
- 29:04 but I know it will come out to a pragmatic place.
- 29:08 [BECKY ANDERSON] Well, that's good to hear.
- 29:09 And I hope you will join us on.
- 29:16 Please go ahead.
- 29:18 [TEDROS ADHANOM GHEBREYESUS] Thank you.
- 29:19 So, on the IP,
- 29:23 I think the IP waiver would be very important.
- 29:27 And as global community, we should ask ourselves,
- 29:31 why do we have even the IP waiver as a legal instrument
- 29:35 if we're not going to use it in such unprecedented conditions?
- 29:39 Insufficient.
- 29:41 This pandemic happened more than 100 years after the 1918 flu.
- 29:48 The provision in the TRIPS Agreement was made in order to use it
- 29:55 in such situations, in emergencies.
- 29:58 So how can we say this should be an issue for debate?
- 30:06 When are we going to use the provision
- 30:10 if we cannot use it now?
- 30:13 My response is we should use the IP waiver now.
- 30:18 We should waive it because these are unprecedented times.
- 30:22 The other thing I would like to raise here is
- 30:25 we have spoken to some countries
- 30:28 who are not supporting the IP waiver
- 30:31 and spoken to manufacturers,
- 30:33 their responses is even if we waive the IP,
- 30:36 it will not be useful unless it's accompanied
- 30:39 by technology transfer.
- 30:41 Our response was,
- 30:43 “Okay, if what you're saying is the problem,
- 30:46 why don't you just waive and let's try if it works or not.”
- 30:52 Without trying you, you wouldn't know.
- 30:56 When you talk about technology transfer,
- 30:59 once you open or waive the IP, it can trigger technology transfer.
- 31:07 Those people who are working for those who control the IP will be free.
- 31:14 Since it will be legalized,
- 31:16 they will be free to migrate and help others,
- 31:19 or they can work part-time to transfer technology.
- 31:24 So it can happen if the IP is waived.
- 31:27 The other is, as Ngozi said, I fully agree,
- 31:32 we need incentives for the private sector.
- 31:35 We need to appreciate their role
- 31:37 because they have developed these vaccines in less than a year.
- 31:41 So in order not to affect the incentives for the long term,
- 31:47 the waiver could be for a very limited period of time.
- 31:50 It could be two years or three years
- 31:52 or until the end of the pandemic.
- 31:54 and it could focus on vaccines only.
- 31:57 But not waiving it now--
- 32:00 [BECKY ANDERSON] I understand.
- 32:01 [TEDROS ADHANOM GHEBREYESUS] when the situation is unprecedented,
- 32:03 the emergency is clear,
- 32:06 and the whole world is the hostage of this virus,
- 32:10 if we cannot waive it now then when.
- 32:12 To be honest, this is really something
- 32:16 where I can say humanity is failing miserably.
- 32:21 This is not acceptable.
- 32:23 It is in the interest of the manufacturers.
- 32:26 It's in the interest of each and every country
- 32:29 in the world to waive the IP,
- 32:31 do everything to increase production,
- 32:34 end this pandemic as soon as possible
- 32:36 and open up the world and release.
- 32:39 [BECKY ANDERSON] You heard that from the head of the WHO.
- 32:44 [NGOZI OKONJO-IWEALA] Can I just add to them just quickly.
- 32:48 We've been talking about waiving these IPs,
- 32:52 and I think that has brought people to the table.
- 32:55 I think let us see in a short while, hopefully maybe,
- 33:00 by our 12th Ministerial, which starts at the end of November,
- 33:05 both sides are talking to each other
- 33:07 and they should come up with a solution
- 33:09 that will give us light on this problem.
- 33:11 [BECKY ANDERSON] Let's hope that happens, Ngozi.
- 33:15 Go on Kristalina.
- 33:16 [KRISTALINA GEORGIEVA] If I may, just to say that
- 33:19 that touched on something very important.
- 33:21 It is the waiver, but then it is the technology ,
- 33:24 it is the skills and the capacity
- 33:26 to build that self-reliance,
- 33:29 and they have to all go hand in hand.
- 33:32 I'm actually encouraged to listen to some of the scientists
- 33:36 and some of the manufacturers that are recognizing
- 33:41 this is a terrible pandemic may not be the last one,
- 33:45 and if the world is to build strength, capacity
- 33:50 to face health risks in the future,
- 33:54 now is the time to approach this in a comprehensive manner.
- 33:59 We need resilience.
- 34:01 We need resilience for shocks to come.
- 34:03 [BECKY ANDERSON] I do want to talk about
- 34:05 that preparedness with all of you.
- 34:09 As we close out this extremely interesting session tonight,
- 34:15 before I do that,
- 34:17 it will come as no surprise to any of you
- 34:20 that we are not only dealing with the pandemic,
- 34:22 but also an infodemic
- 34:25 and a low level of trust in big societal institutions
- 34:29 such as the ones you are leading.
- 34:32 Kristalina, I'm going to start with you because just last night,
- 34:35 the IMF Board affirmed it's full confidence in your leadership,
- 34:39 after investigating your conduct while at the World Bank
- 34:43 related to data regarding China's economic performance.
- 34:47 I want to give you an opportunity
- 34:49 to respond to that decision
- 34:52 and ask you whether you think this episode
- 34:55 has further eroded trust in institutions such as the IMF
- 34:59 and entangled you personally
- 35:02 in the wider geopolitical rivalry between the US and China.
- 35:07 [KRISTALINA GEORGIEVA] Becky, I'm so glad you asked.
- 35:12 The Board of the IMF
- 35:16 in a comprehensive and impartial process,
- 35:21 reviewed the evidence,
- 35:22 and it concluded that it has full confidence
- 35:26 in my leadership at the IMF.
- 35:28 So I can rally the fabulous [inaudible] staff of the IMF
- 35:35 work with our partners, those who are on this panel
- 35:38 to address the tough challenges we face.
- 35:42 We talk about the pandemic, we have climate,
- 35:44 we have the issue of inequality, and of course,
- 35:47 I take it to heart that we have to strive always
- 35:52 to demonstrate that what we do
- 35:55 touches positively the lives of people.
- 35:59 And I take pride of what we have done.
- 36:02 The IMF in these two years
- 36:05 to mobilize incredibly strongly to help our members
- 36:07 incredibly strongly to help our members.
- 36:11 And I am confident that you would see the IMF to be
- 36:17 that beacon of integrity of our data and research
- 36:21 as we have always been.
- 36:23 You are right.
- 36:25 We have to always work for the public trust.
- 36:28 That is what they have been doing for 40 years.
- 36:30 [BECKY ANDERSON] And you've been asking for accountability
- 36:33 and transparency tonight on this very panel.
- 36:36 David, I have to come to you.
- 36:37 The credibility of international organizations has been eroded
- 36:41 due to various controversies, not least that of the IMF firm
- 36:46 or the World Bank and the issue that we've just been discussing
- 36:50 with Kristalina.
- 36:51 Does this trust need to be rebuilt, sir?
- 36:54 [DAVID MALPASS] I'm looking forward
- 36:56 to strong collaboration continued with IMF,
- 36:59 with Kristalina, with Ngozi and Tedros.
- 37:03 And one thing I would say
- 37:04 is you have with you today
- 37:07 four really hard working public officials
- 37:12 that are watched every hour every day, every week.
- 37:17 And so we're working hard in order to get the job done.
- 37:23 I know my day is full of chances to try to make a difference
- 37:28 and to help people.
- 37:29 And I look forward to having as much integrity,
- 37:33 accountability in all of those affairs
- 37:35 as we can, World Bank's doing quality research into the future.
- 37:40 And it's vital as part of the development effort.
- 37:43 [BECKY ANDERSON] What are the learnings out of this episode, David?
- 37:48 [DAVID MALPASS] Learning is constantly review
- 37:52 the quality of your products, make them better, build them hard,
- 37:56 and keep focused on getting good development outcomes for countries.
- 38:00 [BECKY ANDERSON] How do we prepare
- 38:02 for future potential crises, Ngozi?
- 38:06 [DAVID MALPASS] And I was going to say
- 38:09 preparedness is a core part of World Bank and of IDA.
- 38:12 We fast-tracked our front, loaded our IDA into the crisis,
- 38:18 and that's been vital
- 38:19 in delivering as many programs as we have.
- 38:22 [BECKY ANDERSON] Ngozi.
- 38:24 [NGOZI OKONJO-IWEALA] Yeah.
- 38:25 Becky, thank you.
- 38:26 Actually, to prepare for the next crises,
- 38:29 I have to tell you, the G20 Finance Ministers
- 38:32 set up a task force to look into this.
- 38:35 And this was coached by myself, by Larry Summers,
- 38:38 and Tharman Shanmugaratnam, the Senior Minister of Singapore.
- 38:44 And we found four major gaps in pandemic preparedness.
- 38:48 We found that there is a gap
- 38:50 in globally networked surveillance and research
- 38:54 to prevent and detect emerging infectious diseases.
- 38:58 We found a second gap in resilient national systems.
- 39:01 That means that our health systems when this happened
- 39:05 were just not prepared both in rich and poor countries.
- 39:08 We found that there was not an adequate supply
- 39:11 of medical tools and counter measures
- 39:14 to deal with this pandemic.
- 39:16 And as we've just been talking
- 39:18 also inequity of access, the world was not prepared
- 39:22 for access to this.
- 39:23 And the last gap was in global governance.
- 39:25 There just wasn't a mechanism to coordinate
- 39:28 all the different organizations, to make sure that funding
- 39:32 came on time,
- 39:33 and that the international financial architecture worked
- 39:36 and there was no organization to really be accountable
- 39:40 for all the outcomes.
- 39:41 We made three recommendations to be prepared,
- 39:44 and I'll be very fast.
- 39:46 One is that increased--
- 39:47 We all have to increase spending domestically to strengthen
- 39:51 our health systems
- 39:52 in low-income countries and middle-income countries,
- 39:55 we've actually suggested one percentage point of GDP extra
- 39:59 in spending over the next five years in order to be prepared.
- 40:04 In addition to this,
- 40:05 we're also saying we need increased international spending
- 40:09 because there's a public good aspect
- 40:11 for managing the pandemic.
- 40:13 We recommend that $75 billion over the next five years,
- 40:17 15 billion a year of which 10 billion
- 40:20 should go into a global health threat fund.
- 40:23 And finally, we've recommended improved global governance,
- 40:27 a global health threat fund,
- 40:30 a global health threat board
- 40:33 that would oversee and coordinate a preparedness
- 40:37 for the next pandemic, and the spending.
- 40:39 [BECKY ANDERSON] Tedros, I do want
- 40:41 to get your perspective.
- 40:42 I've also got a question from an interested audience member
- 40:47 watching this discussion who says
- 40:50 the WHO is at the forefront of global health.
- 40:53 And Renee asks: Will COVID lead to the reform
- 40:57 of management and investment in medical and health research?
- 41:02 [ENDING THE PANDEMIC: THE ROAD TO AN INCLUSIVE RECOVERY]
- 41:05 [TEDROS ADHANOM GHEBREYESUS] The answer is yes, it will.
- 41:08 As I said earlier, this pandemic is unprecedented
- 41:12 and we're documenting all lessons that we need to learn.
- 41:16 Part of it, which Ngozi said
- 41:18 and all these recommendations should be implemented.
- 41:21 I think this will help us if we can learn
- 41:26 from this pandemic properly
- 41:28 and implement the recommendations,
- 41:30 that we'd be different and we can be better prepared.
- 41:34 One thing I would like to add to this is
- 41:36 the Pandemic Treaty will be very important or Pandemic Agreement.
- 41:41 We have seen many challenges
- 41:44 that could have been addressed if we had a framework
- 41:48 or a legal instrument that could guide us.
- 41:51 So that would be very key
- 41:54 by the way, in the change
- 41:56 we will have to prepare the world in a better way.
- 41:58 The Pandemic Treaty or Pandemic Agreement.
- 42:03 [BECKY ANDERSON] Kristalina, finally,
- 42:04 I just wanted to come to you.
- 42:06 You came to the IMF wanting to talk about gender pay parity,
- 42:10 doing more to tackle the climate crisis,
- 42:13 talking more about income equality.
- 42:17 You couldn't have known quite what was coming down the pipe
- 42:22 with regard the COVID pandemic.
- 42:24 You've gone beyond this narrow focus
- 42:28 and adopted a much more,
- 42:29 as some would describe it, holistic approach,
- 42:34 which is exactly what many of us have said that we needed.
- 42:37 I wonder whether, to a certain extent, you feel
- 42:40 as if that, maybe, what got you into hot water recently,
- 42:44 but also just get your perspective on ultimately,
- 42:47 what the learnings are here
- 42:49 to ensure that we are more prepared
- 42:51 for any eventualities going forward.
- 42:54 [KRISTALINA GEORGIEVA] We are living
- 42:56 in a fast changing world, Becky,
- 43:00 and we have to anticipate
- 43:04 what's next.
- 43:05 And then, have the agility
- 43:08 to prevent crises,
- 43:12 to respond quickly,
- 43:14 to target the most vulnerable,
- 43:17 and to do so,
- 43:20 as Ngozi was saying, across the board.
- 43:23 We need to scan the horizon better.
- 43:26 We have to have better monitoring of these risks
- 43:29 and then, the extra capacity is necessary to step up.
- 43:35 But above all, we need to work on countries to have
- 43:40 strong institutions, educated people that are healthy,
- 43:46 capable to adjust to these shocks,
- 43:50 to hear about the agility and capacity
- 43:55 of our planet to absorb these shocks
- 43:59 and to be with institutions everywhere that have the skills
- 44:05 to lead towards
- 44:08 a more sustainable, more equitable future.
- 44:12 What does it mean if you compare with the pandemic?
- 44:15 Who did the pandemic hit the hardest?
- 44:19 People with weak immune systems, the same way countries
- 44:24 with weak institutions, with weak immune systems
- 44:28 get hit hardest.
- 44:30 So working relentlessly to build
- 44:32 that institutional capacity
- 44:35 to have development that gives jobs to people,
- 44:39 makes them able to have good business opportunities.
- 44:44 This is what matters.
- 44:47 To turn it into the language of our conversation today.
- 44:52 Building resilience is about...
- 44:55 People, institutions and our planet.
- 45:00 [BECKY ANDERSON] Having you all with us today
- 45:04 has been extremely important.
- 45:06 I know that the audience listening to this
- 45:09 will have found this incredibly valuable.
- 45:12 And, David, you're right.
- 45:13 All of you are extremely hard workers.
- 45:16 It is so important that the conversation
- 45:21 is out there, that the challenges that you face are clear
- 45:25 and that the goals that you have set yourself
- 45:27 with this multi-leader task force are clear.
- 45:33 And we hope, achievable,
- 45:34 we thank you very much indeed, all of you for joining us today.
- 45:38 It's been fascinating.
- 45:41 And let's hope that we are not talking in 19 months' time
- 45:47 about the very same issue of vaccine inequality
- 45:50 because that would be terrible.
- 45:53 Thank you very much indeed, for joining us today.
- 45:55 All of you. I'm Becky Anderson.
- 45:57 Good night.
- 46:02 [Upbeat Music]
- 46:13 [ANNUAL MEETINGS 2021]
- 46:14 [WORLD BANK GROUP INTERNATIONAL MONETARY FUND]
- 46:16 [ENDING THE PANDEMIC: THE ROAD TO AN INCLUSIVE RECOVERY]
- 46:24 [JULIETTE POWELL, AUTHOR AND BUSINESS COMMENTATOR] And welcome.
- 46:26 We are live from World Bank Group headquarters in Washington, DC.
- 46:31 I'm Juliette Powell and I'll be your host today
- 46:34 as we continue our discussion on how to end
- 46:37 this pandemic of a truly inclusive recovery.
- 46:41 We've just heard from the leaders of the task force.
- 46:43 And over the next half hour,
- 46:45 we'll be digging deeper into some of the issues and asking
- 46:49 what can be done to accelerate access to vaccines
- 46:52 for developing countries,
- 46:53 And how are the private sector and civil society
- 46:57 helping to address this challenge?
- 46:58 We'll be joined by leaders and experts from across the globe.
- 47:02 Here's a quick look ahead.
- 47:05 [Upbeat Music]
- 47:16 [ANNUAL MEETINGS 2021]
- 47:17 [WORLD BANK GROUP INTERNATIONAL MONETARY FUND]
- 47:20 [COMING UP] [ENDING THE PANDEMIC: THE ROAD TO AN INCLUSIVE RECOVERY]
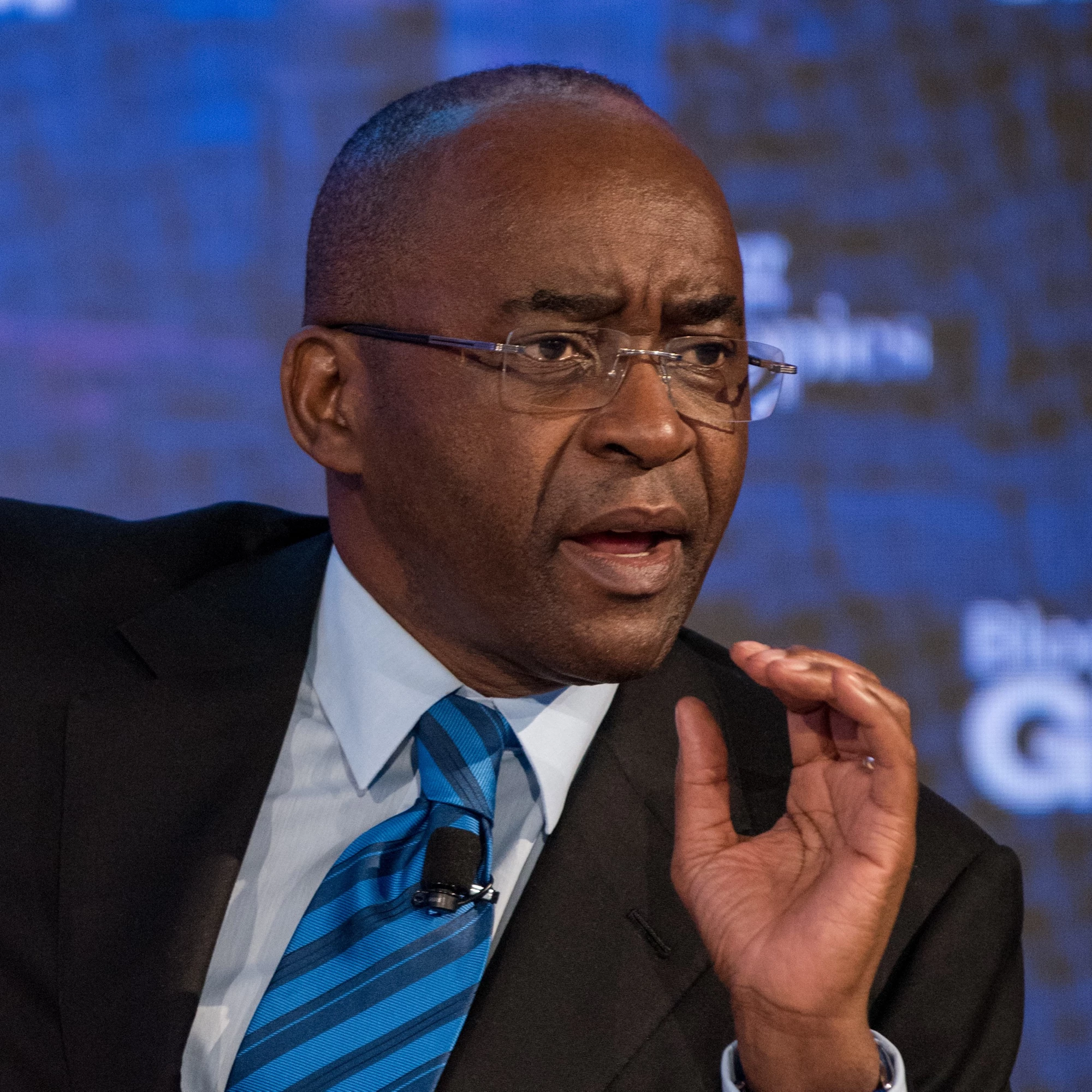
- 47:24 [MAKHTAR DIOP, MANAGING DIRECTOR, IFC]
- 47:26 [NARENDER MANTENA, HEAD OF GLOBAL STRATEGY, BIOLOGICAL E. LIMITED]
- 47:29 [STRIVE MASIYIWA, CHAIRMAN, ECONET & AFRICAN UNION SPECIAL ENVOY]
- 47:33 [DR. AHMED OGWELL OUMA DEPUTY DIRECTOR, AFRICA CDC]
- 47:40 [NADIA DAAR, OXFAM, WASHINGTON DC]
- 47:42 [PRISCILLA NYAABA, YOUTH HARVEST FOUNDATION, GHANA]
- 47:47 [MAMTA MURTHI, VICE PRESIDENT HUMAN DEVELOPMENT, WORLD BANK]
- 47:50 [STEPHANIE VON FRIEDEBURG, SENIOR VICE PRESIDENT OPERATIONS, IFC]
- 47:56 [JULIETTE POWELL] Every single one of us
- 47:58 has been affected by this pandemic and getting through it is
- 48:01 a shared global priority and our responsibility.
- 48:04 We're hearing from people affected in different ways
- 48:07 from youth, civil society organizations
- 48:10 as well as global leaders.
- 48:12 So let's start in the Philippines.
- 48:13 Like in most places, the pandemic shut down schools, markets,
- 48:18 transportation, leaving people desperate
- 48:20 for an end to the threat of COVID-19.
- 48:23 We asked one mother and daughter to share their experiences
- 48:26 and their hopes,
- 48:28 now that vaccines have begun to reach those most in need.
- 48:33 [ANNUAL MEETINGS 2021 WASHINGTON DC]
- 48:36 [Upbeat Music]
- 48:42 The World Bank Group is funding 13 million doses
- 48:44 of COVID-19 vaccine for the Philippines
- 48:47 The first batch arrived in June 2021
- 48:48 with the rest expected by the end of the year.
- 48:51 [DAUGHTER] On TV, in the news, on the internet, they said ta lot of people were dying because of this sickness
- 48:59 And that's what scared us.
- 49:01 [MOTHER] Of course, I was scared - that my kids would get it, my grandchildren would get it, especially us, we're older
- 49:08 [DAUGHTER] Our school announced enrolment would be online instead.
- 49:12 Our internet connection wasn't that strong and their website
- 49:17 kept crashing so I couldn't enrol properly.
- 49:20 There have been so many challenges.
- 49:21 I also couldn't work because there were no rides, I couldn't commute, there was no transportation.
- 49:31 Mom and dad also stopped working then,
- 49:35 [MOTHER] My job was to take care of kids, before when there was no pandemic.
- 49:41 But now, not anymore, because their parents weren't going to work.
- 49:46 -It was hard to know how we'd feed ourselves.
- 49:51 [Upbeat Music]
- 49:57 The World Bank Group is funding 13 million doses
- 49:59 of COVID-19 vaccine for the Philippines
- 50:01 The first batch arrived in June 2021
- 50:03 with the rest expected by the end of the year.
- 50:06 [DAUGHTER] I'm happy mom is vaccinated now. It's her first dose.
- 50:09 She had doubts at first but my sister and I told her that side effects are normal.
- 50:16 [MOTHER] I'm OK now. I'm happy because my children have work and I've also been vaccinated.
- 50:21 My husband has work too.
- 50:23 Things are not as hard for us anymore.
- 50:25 [DAUGHTER] My dream is to finish studying, to keep going without having to stop.
- 50:32 And then to become an HR manager. That's what I really want.
- 50:37 The World Bank Group is boosting private sector vaccine manufacturing capacity globally.
- 50:40 [DAUGHTER] I'm happy that (vaccines) have arrived in the Philippines.
- 50:43 Some people have already been vaccinated and it keeps going
- 50:46 What I want to say is that I hope we can speed up vaccination efforts
- 50:52 so we can end this difficult pandemic
- 50:56 and we can continue
- 51:00 chasing our dreams.
- 51:04 #vaccines4all
- 51:11 [ANNUAL MEETINGS 2021 WASHINGTON DC]
- 51:13 [WOMAN] Salam. I'm [inaudible] from Almaty, and you are watching
- 51:18 the World Bank Group-IMF Annual Meeting.
- 51:24 [JULIETTE POWELL] What an incredible story of survival and hope.
- 51:27 We're streaming this event
- 51:29 in English, French, Spanish and Arabic on World Bank Live
- 51:33 and on our social media channels and to tell us
- 51:36 how you can finally get involved,
- 51:38 I'm joined now by Sri Sridhar. Welcome, Sri.
- 51:41 [SRI SRIDHAR] Thanks, Juliette.
- 51:42 [JULIETTE POWELL] So we had a chance to listen
- 51:44 to the task force leaders talking about all of those challenges.
- 51:47 How about getting the people that are watching involved as well?
- 51:50 [SRI SRIDHAR] Absolutely.
- 51:51 So similar to yesterday, you can follow us
- 51:53 on our social media channels.
- 51:54 We're on Facebook, Twitter, and Instagram.
- 51:57 You can also share comments at any time
- 51:59 using the hashtag for today's event, which is #vaccinesforall.
- 52:02 And you can also post your questions and comments
- 52:04 at any time on live.worldbank.org.
- 52:07 So really a lot of ways for everyone
- 52:09 to kind of get involved and join the conversation.
- 52:11 Now, you did mention that the event is being streamed
- 52:13 in English, Spanish, French and Arabic.
- 52:15 And the good news is we've got
- 52:17 experts standing by in all four languages,
- 52:19 and they're working hard to answer as many questions as possible.
- 52:22 We can see some of them right here.
- 52:24 And I know that some of the most popular questions
- 52:27 I think are gonna be put to a couple of the senior experts
- 52:29 later today.
- 52:30 [JULIETTE POWELL] Yeah, we're very, very lucky.
- 52:31 We're gonna be joined a little bit later on by Mamta Murthi
- 52:35 He's the Bank's Vice President of Human Development.
- 52:38 We've also got Stephanie von Friedeburg.
- 52:40 She-- You might even know her.
- 52:42 She's a Senior Vice President of Operations for IFC,
- 52:45 and we've got our viewers.
- 52:47 Now, how do we get them involved in the poll?
- 52:49 [SRI SRIDHAR] Yeah. So the poll for today asks:
- 52:52 What is most important to ensure equitable
- 52:55 and successful COVID-19 vaccine deployment?
- 52:58 And there are four options.
- 53:00 The first, is it by having an adequate stock of vaccines?
- 53:03 A sufficiently funded, resilient and inclusive health system.
- 53:07 Enough equipment and trained public health personnel? Or is it
- 53:10 by having engagement of local community leaders and organizations?
- 53:15 So once again, the poll for today asks:
- 53:17 What is most important to ensure equitable
- 53:19 and successful COVID-19 vaccine deployment.
- 53:22 And the choices are by having an adequate stock of vaccines.
- 53:26 A sufficiently funded, resilient and inclusive health system.
- 53:30 Enough equipment and trained public health personnel, or
- 53:33 is it engagement of local community leaders and organizations?
- 53:36 So for those of you folks who are tuning in head on over
- 53:39 to live.worldbank.org and cast your vote before the poll closes.
- 53:43 [JULIETTE POWELL] Thanks so much Sri.
- 53:44 I really look forward to hearing what the results are going to be.
- 53:47 We're gonna find out by the end of the show today.
- 53:50 -Thanks. -Thanks, Juliette.
- 53:54 [JULIETTE POWELL] Now the private sector is playing a very
- 53:57 important role in pandemic response,
- 53:59 vaccine production and distribution.
- 54:01 To learn more about what the private sector
- 54:04 can and is doing to meet vaccine needs,
- 54:07 and the challenges faced
- 54:08 IFC Manager Director, Makthar Diop, is joined
- 54:11 in discussion by two leaders in the health field.
- 54:14 [MAKTHAR DIOP] I'm joined by two great leaders
- 54:17 who are in the area, each making a huge difference.
- 54:21 Strive Masiyiwa is a founder of Econet
- 54:25 a leader company in the mobile-- digital sector in Africa
- 54:30 but also he's-- he has been working
- 54:32 a lot on vaccine, and he's a Special Envoy
- 54:34 from the African Union to help really bring
- 54:37 the private sector in producing more vaccine in Africa.
- 54:40 Narender is a CEO of [inaudible].
- 54:43 Well, as you know, a lot of the production
- 54:45 of vaccine has been coming from India and the research
- 54:48 also in this area has been going on.
- 54:50 We have today's situation
- 54:53 where only 4% of the population in Africa is vaccinated.
- 54:56 We have a lot of vaccine inequity
- 54:59 that has been discussed and talked about.
- 55:01 And today we would like to discuss
- 55:03 what we can do to solve that issue.
- 55:05 And these two leaders,
- 55:06 will give us the insight and the idea
- 55:09 about how we can go about it.
- 55:11 Let me start first with Strive.
- 55:14 So have you been involved very much in making
- 55:18 sure that we increase the supply of vaccine in Africa.
- 55:22 So what needs to be done
- 55:24 to increase the supply of vaccine in Africa?
- 55:27 [STRIVE MASIYIWA] Thank you very much, Makhtar.
- 55:29 It's good to see you, my dear brother.
- 55:31 My job as the African Union Special Envoy
- 55:36 is to coordinate the acquisition of vaccines.
- 55:40 My primary-- I
- 55:43 I coordinate the task force made up of ministers
- 55:47 and health specialists,
- 55:50 including the Africa Center for Disease Control,
- 55:54 to purchase vaccines.
- 55:57 We have created a special purpose vehicle called
- 56:01 the Africa Vaccine Acquisition Trust,
- 56:05 which we funded
- 56:08 with a 2 billion dollar facility.
- 56:13 We also have secured, as you know,
- 56:17 over 4 billion dollars of support from the World Bank
- 56:21 for the member states to buy vaccines.
- 56:23 This is the first time anything of this scale
- 56:27 has ever been done where Africa is buying together
- 56:31 vaccines on a major scale.
- 56:34 So I've gotta-- Although I don't come from the sector,
- 56:38 I've picked up some idea what the challenges are,
- 56:41 and I hope we'll be able to discuss them as we proceed
- 56:47 But really, that is my job.
- 56:51 And it's been-- The challenge for us
- 56:55 has been to secure supply
- 56:58 because Africa made the mistake
- 57:02 of seeding manufacturing of vaccines
- 57:06 to other regions of the world.
- 57:08 And this is the thing that we have to fix,
- 57:11 that vaccines must be manufactured on the African soil.
- 57:16 [MAKHTAR DIOP] Thank you very much, Strive.
- 57:18 I come back to you and ask you, what are the conditions
- 57:21 for it to happen?
- 57:22 And with your huge experience in the private sector
- 57:27 in Africa, what needs to be done to attract private sector in vaccine?
- 57:31 I'll come back to you to that after I ask Narender
- 57:34 who is from India, where had they been able to do that?
- 57:37 So how have we been able to do that in India?
- 57:41 And what are the three lessons
- 57:43 that you can draw from your experience
- 57:46 such-- can be useful
- 57:47 for the part of the world who wants to do the same thing.
- 57:49 [NARENDER MANTENA] And India is a different story.
- 57:53 I think it's a long story. And quickly...
- 57:56 The Indian private sector manufacturing started in the 60s
- 58:00 with the Serum Institute in our company in a small way.
- 58:03 But the real [inaudible] for the Indian vaccine manufacturing
- 58:06 didn't happen until Gavi was formed
- 58:09 in the late 90s and 2000s,
- 58:12 there were incentives created by the Gates Foundation in WHO
- 58:17 to prequalify companies out of India,
- 58:20 and they started supplying the global market
- 58:22 that included Africa and other nations.
- 58:25 I think that gave the [inaudible]
- 58:28 of large capacities in India
- 58:30 that we're able to utilize now.
- 58:34 On top of that, India also had large biologics,
- 58:38 and biosimilar market, and these facilities have been repurposed.
- 58:43 So I think it's not one simple story.
- 58:46 It is a combination of an evolution of a domestic market
- 58:51 incentivized by global markets in UNICEF and Gavi,
- 58:55 and complemented with the pharmaceutical markets
- 58:58 that allowed India to be able to respond to the pandemic
- 59:01 in its own way.
- 59:02 In terms of lessons, I think that this lesson is
- 59:06 probably not the right way to go
- 59:08 because it takes a long time to get there,
- 59:10 and I'm sure Strive will talk about it.
- 59:12 But-- continents like Africa
- 59:16 do have the ability to create a market of its own
- 59:20 and by centralized procurement
- 59:23 to incentivize manufacturers to come into Africa.
- 59:26 I think the challenge of the pandemic is
- 59:28 slightly different, because if you look at how the pandemic
- 59:32 has been addressed, not only in India but in US and Europe,
- 59:37 they had to leverage pharmaceutical facilities
- 59:39 to be able to scale up.
- 59:41 So...
- 59:42 creating a pandemic-ready infrastructure
- 59:45 will be a different challenge that we have to figure out
- 59:48 how to address.
- 59:50 So I think the three lessons would be domestic market
- 59:54 for Africa, for African manufacturers
- 59:58 incentivizing either with a push and pull funding
- 01:00:02 to make the prices affordable and to create
- 01:00:06 pandemic manufacturing infrastructure
- 01:00:09 and funding it on a regular basis.
- 01:00:11 Not knowing when the next pandemic will hit
- 01:00:14 would be the lessons, they're not directly from India.
- 01:00:17 But India was able to do it organically.
- 01:00:20 But that's what I believe needs to be done in other areas.
- 01:00:24 [MAKHTAR DIOP] Thank you very much.
- 01:00:25 Let me turn to my friend Strive.
- 01:00:27 So having been one as a precursor in an area
- 01:00:30 where this was quite complicated at the beginning, digital.
- 01:00:33 Not a lot of people wanted to put their money in Africa
- 01:00:36 take that risk and be able to price the risk,
- 01:00:39 understanding and to be able to address the challenges
- 01:00:42 that people-- investors were facing at that time.
- 01:00:46 Build on your experience in the digital, what you think,
- 01:00:51 from what you heard from Narender, from your own experience
- 01:00:55 will be the condition to attract more private investment
- 01:00:58 in vaccine, in Africa.
- 01:01:01 [STRIVE MASIYIWA] Well, you know, I think
- 01:01:04 it's very important what my colleague just said,
- 01:01:09 it's very profound
- 01:01:12 because I came to the same conclusion.
- 01:01:16 But it was institutions like Gavi
- 01:01:20 that are responsible for the crisis in Africa
- 01:01:26 because what they did was to create
- 01:01:28 a public market in the purchase of vaccines
- 01:01:33 and then to strategically shift it to India.
- 01:01:36 So there is no way that African industrialists
- 01:01:40 could respond because the buyer--
- 01:01:44 decided that Africa's vaccines would come from India.
- 01:01:49 This was a strategic decision
- 01:01:53 in which Africans had no say.
- 01:01:57 And so we find ourselves in this situation
- 01:02:00 whereby when we found-- when we got into a crisis
- 01:02:04 and India was in the same crisis,
- 01:02:07 India said it would take care of its own people
- 01:02:12 and we went to the back of the queue.
- 01:02:15 Africans are really mad about this.
- 01:02:18 Okay?
- 01:02:19 And I have told Gavi and UNICEF and even Gates
- 01:02:24 that this was wrong.
- 01:02:25 We need to correct this.
- 01:02:28 I'm sorry, but we got a big blunt about it.
- 01:02:31 African industrialists can do exactly what Indian industrialists can do.
- 01:02:35 Okay?
- 01:02:37 We have companies in Africa who were denied
- 01:02:40 the opportunities that were extended
- 01:02:43 to Indian manufacturers,
- 01:02:44 and that's why we're in this mess.
- 01:02:47 And we have to correct it.
- 01:02:50 We admire what has happened in India,
- 01:02:52 but we have to do the same
- 01:02:54 because we exported to India millions of jobs
- 01:02:59 in the production of vaccines.
- 01:03:01 Okay?
- 01:03:02 And I have said this and I will say it again.
- 01:03:05 We have to fix it.
- 01:03:08 How industrialists are capable of producing vaccines.
- 01:03:14 This is not a complicated thing.
- 01:03:16 It's the same technology that they have access to.
- 01:03:20 We know from Aspen
- 01:03:23 and Biovac and Dakar Institute
- 01:03:27 that had the same support
- 01:03:30 being given to them by the likes of Gavi and UNICEF,
- 01:03:35 we would not be in this mess.
- 01:03:38 So I will say it and say it again.
- 01:03:42 [MAKHTAR DIOP] So, I thank you very much.
- 01:03:43 But I think that there is an opportunity for convergence here.
- 01:03:47 And Narender, I know that you are looking also
- 01:03:50 at working in other places outside from India.
- 01:03:55 And I think, maybe, this is an opportunity
- 01:03:58 to invest in Africa because there is need,
- 01:04:02 there is a market, as you said, and there is a willingness
- 01:04:05 to build that ecosystem in some of the countries.
- 01:04:08 Would you be interested
- 01:04:09 if industrialists from Africa, as I've said, were approaching you
- 01:04:15 and said, let's do a joint venture, and invest on the continent?
- 01:04:19 [NARENDER MANTENA] Absolutely.
- 01:04:21 I think for us.
- 01:04:22 And as I said, I think that I completely agree with Strive
- 01:04:28 on the outcome of what Gavi did with respect to the pandemic.
- 01:04:32 Now, whether Gavi could have foresaw it
- 01:04:34 this kind of a pandemic. I mean, that's debatable.
- 01:04:38 I think we have never--
- 01:04:39 the world has never seen a pandemic like this.
- 01:04:41 Where essentially everybody had to get vaccinated.
- 01:04:45 So having said that to answer your question,
- 01:04:48 I think we definitely look at Africa.
- 01:04:50 I think for us, you know...
- 01:04:53 It is a market of importance we have been servicing through Gavi
- 01:04:57 but if it necessitates-- not necessitates-- It is.
- 01:05:02 The pandemic has taught us that,
- 01:05:05 you know, while we appreciate India looking out for India,
- 01:05:09 as a private company,
- 01:05:11 we don't feel good when people that have supported us globally,
- 01:05:16 that is [inaudible], Africa.
- 01:05:17 We're not able to service.
- 01:05:19 So it's not a good feeling
- 01:05:21 when you are not able to give back to countries
- 01:05:24 that have supported us for a long time.
- 01:05:26 But unfortunately, it's not in our hands
- 01:05:29 but to answer your question, yes, I think that we would be very open
- 01:05:31 as a company to do it ourselves.
- 01:05:34 Our preference is to find partners that we can do it with,
- 01:05:37 and then we'd be very open, and we're in fact, actually,
- 01:05:39 where we are slowly initiating discussions around it.
- 01:05:43 [MAKHTAR DIOP] I think that this conversation
- 01:05:46 was aiming at creating this link.
- 01:05:49 And I think that we are building it together, the three of us.
- 01:05:52 So, Strive to you, please.
- 01:05:53 [STRIVE MASIYIWA] Well, when I met with you, recall,
- 01:05:57 I said the future for you
- 01:06:00 is to manufacture from Africa.
- 01:06:03 You can own a hundred percent.
- 01:06:06 I will personally buy, you name the African country.
- 01:06:10 I'll buy the land and give it to you for free
- 01:06:12 myself with my own money.
- 01:06:14 Okay?
- 01:06:15 As a gift, you must manufacture from Africa.
- 01:06:19 And the future.
- 01:06:21 Is that's what's going to happen
- 01:06:23 When Sinophone came to me, I said you manufacture from Africa.
- 01:06:28 Otherwise, you don't get orders.
- 01:06:29 They are now manufacturing in Africa.
- 01:06:32 I'll give them an order.
- 01:06:33 If you want orders from us as AVAT,
- 01:06:36 you come and manufacture from Africa,
- 01:06:38 you choose your country, you do what you want.
- 01:06:41 You can have it a hundred percent whatever you want.
- 01:06:45 But you do it from Africa.
- 01:06:46 And we are going to start putting a lot of pressure on Gavi.
- 01:06:51 Every single contract that Gabi now signs.
- 01:06:55 If it is to supply Africa,
- 01:06:57 they must justify
- 01:07:00 where that-- why that production did not come from Africa.
- 01:07:04 Okay. It's-- It's going--
- 01:07:06 This is the result
- 01:07:08 of the decision that was taken in India to just cut us off.
- 01:07:13 You cut us off in March.
- 01:07:14 Politically, they said no more vaccines.
- 01:07:17 We'll deliver to you when we have delivered to our own people,
- 01:07:21 which is what Europe did to us.
- 01:07:24 Okay, so we've-- I've said it to the Indian manufacturers.
- 01:07:28 You are welcome.
- 01:07:30 You, Serum Institute, buyer.
- 01:07:32 Come, come.
- 01:07:34 But you make from Africa, so we can also have jobs.
- 01:07:38 And next time, no one can cut us off politically.
- 01:07:42 [MAKHTAR DIOP] Thank you so very much, my friend.
- 01:07:44 This is a wonderful conversation.
- 01:07:46 But unfortunately, as I say,
- 01:07:48 in my country every good-- all good things have an end.
- 01:07:51 and we have, too.
- 01:07:52 But I think that we made a lot of progress, Strive and Narender,
- 01:07:55 thank you very much.
- 01:07:57 Often we say, as these discussions, meetings leading to something.
- 01:08:01 Today, I have the feeling
- 01:08:02 that it leads to something very concrete and precise.
- 01:08:04 Strive you made a call for investment,
- 01:08:07 investing in Africa.
- 01:08:09 Narender says yes. "I'm looking at it."
- 01:08:11 "I'm interested in doing that."
- 01:08:13 So I think that IFC would be working with both of you
- 01:08:17 we'd be very happy to be your partner in doing
- 01:08:20 that together and creating those opportunities.
- 01:08:24 So this is for us, a great outcome of the conversation.
- 01:08:28 And we continue and let me say a last word.
- 01:08:31 This is just the beginning for us
- 01:08:34 of investing in the highest sector in Africa.
- 01:08:37 We have a lot of other health challenges to deal with.
- 01:08:40 Diabetes is becoming an increasing problem in Africa.
- 01:08:44 I brought pressure.
- 01:08:45 All these drugs, which are so necessary to improve
- 01:08:48 the half of African population,
- 01:08:50 need to be built cheaply,
- 01:08:52 make it accessible to people of Africa.
- 01:08:55 But I think that this conversation that we started,
- 01:08:57 for me, is the beginning of a bright future.
- 01:09:01 And I would like to thank you for joining me.
- 01:09:04 -Yes, please, Strive. -[STRIVE MASIYIWA] Let me just say one quick thing.
- 01:09:07 I'm not in the vaccine industry.
- 01:09:09 I'm a tech guy.
- 01:09:11 Okay?
- 01:09:12 I will help you find partners if you want.
- 01:09:15 You can be a hundred percent.
- 01:09:17 You are welcome.
- 01:09:18 Come and produce in Africa.
- 01:09:21 [MAKHTAR DIOP] Beautiful word to conclude, Strive.
- 01:09:23 Thank you so much, all of you.
- 01:09:25 And be safe.
- 01:09:27 Thank you so much.
- 01:09:30 [MAN] Hi, I'm [inaudible] from Dhaka.
- 01:09:32 And you're watching the World Bank Group-IMF Annual Meetings
- 01:09:37 [JULIETTE POWELL] If you're just joining us, I'm Juliette Powell.
- 01:09:41 And you're watching
- 01:09:42 Ending the Pandemic: The Road to an Inclusive Recovery.
- 01:09:45 It's been incredible.
- 01:09:47 Listening to Makhtar and his guests discuss
- 01:09:49 the vaccine challenge in Africa.
- 01:09:51 Now, we all know that the situation varies across the continent,
- 01:09:54 but on average,
- 01:09:56 less than five percent of the African population
- 01:09:59 is vaccinated, and that's why the World Bank
- 01:10:01 has intensified its technical and financial support in the region.
- 01:10:05 So let's take a look at how that's actually making a difference
- 01:10:08 to the health systems
- 01:10:10 and particularly, for the people in Cote d'Ivoire.
- 01:10:14 [ANNUAL MEETINGS 2021 WASHINGTON DC]
- 01:10:17 When COVID-19 hit Africa, healthcare systems struggled to cope
- 01:10:25 [WOMAN] At the beginning of the pandemic,
- 01:10:27 it was very difficult for ourselves, as health care personnel
- 01:10:32 in our relationships with our relatives, friends, clients, and staff,
- 01:10:39 given the fact that the disease, it's very contagious
- 01:10:43 In Cote d'Ivoire the World Bank Group supported a program that is:
- 01:10:47 Operating mobile clinics, deploying vaccines in 113 health districts
- 01:10:50 diversifying vaccine supply sources, raising awareness.
- 01:10:53 [MAN] Like most people,
- 01:10:54 I sensed that there was a slowdown across the board in 2020.
- 01:11:02 I even had to stay with my children for some time to teach them at home
- 01:11:07 Then, on top of that, there are all these stories that you hear from other people, and reports from various sources
- 01:11:14 and from the media.
- 01:11:16 So, once I realized the gravity of the situation I decided to go and get the vaccine
- 01:11:23 Within 4 weeks, the number of people vaccinated increased ten-fold
- 01:11:29 Giving people hope for the future
- 01:11:33 [WOMAN] The more people are vaccinated, the faster we will stop the virus from circulating.
- 01:11:40 And then people will start to resume their regular activities,
- 01:11:44 because I'm sure you will agree with me that since the outbreak of the disease there have been so many things that we can no longer do.
- 01:11:50 We need to get back to a normal life.
- 01:11:52 And, for us to do so, for us to start living a normal life again,
- 01:11:56 the vaccine is our only hope.
- 01:11:58 To get through this pandemic and future crises
- 01:12:01 we need stronger health systems to:
- 01:12:02 Improve effective vaccine delivery,
- 01:12:04 be better prepared for future health emergencies
- 01:12:06 support human capital development
- 01:12:09 [ANNUAL MEETINGS 2021 WASHINGTON DC]
- 01:12:11 [JULIETTE POWELL] Combating the pandemic
- 01:12:13 through the successful rollout of vaccination programs
- 01:12:16 requires collaboration across all levels.
- 01:12:19 The African Vaccine Acquisition Trust is a joint initiative between
- 01:12:24 the African Union,
- 01:12:25 he Africa Centers for Disease Control and Prevention
- 01:12:28 the World Bank and other African institutions.
- 01:12:31 And the whole idea is to fast-track
- 01:12:33 vaccine acquisition on the continent.
- 01:12:35 It's being heralded as an extraordinary regional effort
- 01:12:39 and I recently had the opportunity to speak
- 01:12:41 to Dr. Ahmed Ogwell, he's Deputy Director of the Africa CDC
- 01:12:46 about the importance of regional collaboration
- 01:12:49 and all of the challenges faced.
- 01:12:52 I'm joined now by Dr. Ogwell.
- 01:12:54 Let me begin by asking you this,
- 01:12:57 why is such a regional collaboration
- 01:12:59 so crucial in the fight of COVID-19,
- 01:13:02 but also to ensure better preparedness
- 01:13:04 for future health emergencies?
- 01:13:06 [DR AHMED OGWELL OUMA] Thank you for having me.
- 01:13:11 Collaboration within a region is very crucial,
- 01:13:14 and this is because
- 01:13:16 these countries and communities are neighbors,
- 01:13:19 they share the same, similar circumstances.
- 01:13:24 They share similar cultures and understanding.
- 01:13:28 Very often, they also share very similar capacities,
- 01:13:32 whether it is technical, knowledge or financial.
- 01:13:36 Leveraging on the expertise that is found within a region
- 01:13:40 is much easier than waiting for expertise
- 01:13:43 to come from far away.
- 01:13:44 Whether it is expertise in terms of knowledge
- 01:13:48 or whether it is equipment and infrastructure
- 01:13:52 in terms of laboratory and similar tools,
- 01:13:57 doing that within a region is so much easier.
- 01:14:01 Most of the regions today
- 01:14:03 are already geopolitically organized
- 01:14:06 into regional economic blocks or regional political blocks.
- 01:14:11 So working within a region like that
- 01:14:14 makes it much easier to gain consensus
- 01:14:17 and then be able to affect some action,
- 01:14:21 especially when it is required quickly.
- 01:14:24 Now, when you look at how do we prepare
- 01:14:28 for future possible health emergencies,
- 01:14:32 you find that regional response is better,
- 01:14:36 because you can quickly be able to share data,
- 01:14:38 you can quickly be able to share experts,
- 01:14:41 you can quickly be able to share resources
- 01:14:43 so that you respond in a very communal manner
- 01:14:47 in a group of countries,
- 01:14:49 and the effect is much faster in that way.
- 01:14:53 Therefore any health risk can be quickly brought under control.
- 01:14:59 [JULIETTE POWELL] The pandemic has highlighted
- 01:15:01 the risk of major disease outbreaks
- 01:15:03 and highlighted many countries'
- 01:15:05 lack of preparedness to fight them.
- 01:15:09 We've all seen the devastated human and economic fallout
- 01:15:13 and toll that this has taken.
- 01:15:15 But the Africa CDC is focusing
- 01:15:17 on disease surveillance, control and prevention,
- 01:15:21 as well as emergency preparedness.
- 01:15:24 Can you please tell us
- 01:15:26 what are the biggest challenges in this work
- 01:15:29 for you professionally and personally.
- 01:15:32 [DR AHMED OGWELL OUMA] Let me list a few.
- 01:15:34 One at the top of my list is supply chain.
- 01:15:38 One big challenge has been
- 01:15:40 how do we get the health products that we need
- 01:15:43 in preparedness and response
- 01:15:46 on to the continent and to ground zero,
- 01:15:50 where the health products are really required.
- 01:15:53 Whether it is as basic as masks,
- 01:15:55 or it is as complex as vaccines,
- 01:15:58 how do we secure that supply chain?
- 01:16:00 Africa is not manufacturing enough
- 01:16:02 of its own health products,
- 01:16:04 and this has been a huge challenge.
- 01:16:06 Something that we must address going into the future.
- 01:16:09 Second, is insufficient regulatory capacity
- 01:16:14 when you are bringing in health products of any type,
- 01:16:17 whether it's medicines, vaccines, diagnostics,
- 01:16:21 you want a regulatory system that works, and works quickly.
- 01:16:25 Now, Africa's regulatory system is not as strong,
- 01:16:28 and this is something that we need to build very quickly.
- 01:16:32 Third is workforce.
- 01:16:34 Where are those experts?
- 01:16:35 How many do you have?
- 01:16:37 How can you distribute them across the continent?
- 01:16:39 This has been a big challenge, because we don't have enough.
- 01:16:42 As widespread as nurses are,
- 01:16:47 they're not enough on the continent.
- 01:16:50 As few as epidemiologists,
- 01:16:51 the disease intelligence officers are,
- 01:16:53 they are very few on the continent
- 01:16:55 and everything in between.
- 01:16:56 So work force is a very critical challenge that we are facing.
- 01:17:00 Fourth are institutions.
- 01:17:02 Do you have institutions at country level
- 01:17:05 that can be able to guide preparedness and response?
- 01:17:08 Do you have institutions
- 01:17:09 at the continental level that are able to do that?
- 01:17:12 Well, luckily, at the continental level,
- 01:17:13 Africa cities there and we've been doing
- 01:17:15 a lot of this coordination,
- 01:17:17 but at country level, there are still gaps.
- 01:17:19 So I would say that these are
- 01:17:21 the four main challenges that we see
- 01:17:23 as far as preparedness and response is concerned.
- 01:17:27 An overarching challenge is the public.
- 01:17:31 How do you get the correct information to them?
- 01:17:34 And how do they respond to that correct information
- 01:17:37 in the middle of an avalanche of fake news
- 01:17:40 and half truths that are being pedaled in social media?
- 01:17:44 So this is a very overarching challenge,
- 01:17:47 in respect of what kind of outbreak
- 01:17:49 or health emergency we may be responding to.
- 01:17:52 Just prior to the COVID-19 pandemic,
- 01:17:55 the World Bank funded
- 01:17:57 the Africa CBC Regional Investment Financing Project.
- 01:18:00 The idea was to strengthen disease surveillance,
- 01:18:04 prevention and emergency response systems
- 01:18:06 across the African continent.
- 01:18:08 How is that kind of support,
- 01:18:10 from the World Bank and other institutions,
- 01:18:13 help the Africa CDC to grow over the past years,
- 01:18:16 and more to the point, what's next?
- 01:18:19 The World Bank has been a very good partner.
- 01:18:23 They came through for Africa CDC
- 01:18:27 at the beginning of the establishment of the agency
- 01:18:32 and supported us in three big ways.
- 01:18:36 One was to strengthen Africa CDC internally.
- 01:18:40 Our capacity, staffing.
- 01:18:44 This has been supported very effectively.
- 01:18:46 Second, is to strengthen
- 01:18:48 our ability to build our regional surveillance
- 01:18:53 and laboratory networks. We call that RISLNET.
- 01:18:56 This is where we bring together all the resources in a region,
- 01:19:00 so that they are working for a region
- 01:19:03 and not only for a country.
- 01:19:05 And that particulary, granted others,
- 01:19:07 has continued to help our work.
- 01:19:10 And third, is to build the capability
- 01:19:13 of Africa CDC to support our member States on the continent.
- 01:19:18 This is in many ways to build a capacity of the member States
- 01:19:23 and as well as to provide much needed infrastructure
- 01:19:27 for preparedeness and response.
- 01:19:29 Now, when we look into the future,
- 01:19:32 we are proposing that Africa CDC's new public health order
- 01:19:36 needs to be supported and implemented
- 01:19:39 so that we can effectively be able to prepare and respond
- 01:19:44 to health emergencies on the continent.
- 01:19:46 The new public health order has four plans.
- 01:19:50 One is strengthening institutions
- 01:19:52 for public health emergencies on the continent.
- 01:19:54 Both are the continental and national levels.
- 01:19:57 Second, is building the capacity of our workforce
- 01:20:01 that we require to respond to health emergencies.
- 01:20:05 Third, is local manufacturing of all the products that we need
- 01:20:10 from those are simple as masks
- 01:20:12 to those that are complex as vaccines.
- 01:20:14 We need to secure the supply chain on the continent.
- 01:20:17 And the fourth pillar is action oriented
- 01:20:20 and respectful partnerships
- 01:20:22 that are based on the priorities of Africa.
- 01:20:26 If we support the implementation of the new public health order,
- 01:20:30 Africa would be better prepared
- 01:20:31 for the next pandemic or the next outbreak.
- 01:20:34 [JULIETTE POWELL] Thank you so much, Dr. Ogwell.
- 01:20:36 It has been a joy to listen to you today.
- 01:20:39 It has been incredibly inspiring,
- 01:20:41 and we are very thankful for your time.
- 01:20:44 Thank you.
- 01:20:46 [WOMAN] Manao ahoana. I am [inaudible] from Madagascar
- 01:20:48 and you're watching the World Bank-IMF Annual Meetings.
- 01:20:54 [JULIETTE POWELL] How important to be reminded
- 01:20:56 that strong regional collaboration
- 01:20:58 and the sharing of data, expertise and resources
- 01:21:01 altogether can bring health emergencies
- 01:21:04 under control much more quickly.
- 01:21:06 Equitable access to vaccines is crucial
- 01:21:09 to ending the pandemic everywhere.
- 01:21:11 And we know that access
- 01:21:13 in developing countries remains very limited.
- 01:21:15 We've asked civil society leaders Priscilla Nyaaba,
- 01:21:20 executive director of Youth Harvest Foundation, Ghana,
- 01:21:23 and Nadia Daar.
- 01:21:24 She heads up the Washington D.C. office of Oxfam International
- 01:21:28 to share their thoughts and namely,
- 01:21:30 how limited access is affecting communities
- 01:21:33 and what their organizations are trying to do about it.
- 01:21:39 [PRISCILLA NYAABA] We have a mission
- 01:21:41 to support and empower young people
- 01:21:42 to achieve their full potential
- 01:21:44 in their personal life in their professional development,
- 01:21:47 for them to become active advocates
- 01:21:49 of the rights of young people.
- 01:21:51 Since the onset of COVID-19,
- 01:21:53 the Youth Harvest Foundation in Ghana collaborated
- 01:21:55 with Ghana Help Service
- 01:21:56 to create more awareness about the pandemic.
- 01:21:59 Using community radios,
- 01:22:00 information vans and on our social media platforms,
- 01:22:04 we created the Ghana COVID-19
- 01:22:06 Support Network platform on Facebook.
- 01:22:08 We also made donations of PPEs and other logistics
- 01:22:11 to the Ghana Help servicing the upper each region
- 01:22:14 to help fight the infection.
- 01:22:15 Some of the unforeseen effects
- 01:22:18 of low to no access to COVID-19 vaccines in Ghana
- 01:22:22 and in [inaudible]
- 01:22:24 is the limited access
- 01:22:26 to productive health services information
- 01:22:28 by women and girls, because of fear of being infected.
- 01:22:32 [NADIA DAAR] Low to no access to vaccines is resulting
- 01:22:35 in the world growing even more unequal.
- 01:22:38 Less than 1% of vaccines have gone to low-income countries.
- 01:22:42 26 people in Africa are dying every hour from COVID,
- 01:22:46 as they're told to wait for vaccine charity
- 01:22:48 from wealthy countries.
- 01:22:49 Donations are crucial,
- 01:22:51 but they're neither sustainable nor sufficient.
- 01:22:53 We have to address the monopoly control
- 01:22:56 that a few pharmaceutical corporations
- 01:22:58 have over vaccine price and supply.
- 01:23:01 Oxfam has been working with the People's Vaccine Alliance
- 01:23:04 to secure the temporary waiver
- 01:23:06 of intellectual property rules at the WTO.
- 01:23:08 While many are in favor,
- 01:23:10 we need all governments urgently agree
- 01:23:12 that the rights to produce these vaccines are shared,
- 01:23:15 to ensure the technology to produce them are transferred
- 01:23:18 via the WHO,
- 01:23:19 and that manufacturers around the world
- 01:23:21 have support to make them.
- 01:23:23 And we need the IFIs to use their extraordinary power
- 01:23:26 to help make this happen.
- 01:23:35 [JULIETTE POWELL] And that was a very good reminder
- 01:23:37 of the enormous disruptions in health care
- 01:23:39 that were caused by the pandemic,
- 01:23:41 and the impact that it's had on everyone,
- 01:23:44 even those not directly affected by the disease.
- 01:23:47 Find out more about how the Bank is responding to the pandemic
- 01:23:50 and accelerating vaccine delivery
- 01:23:52 at WorldBank.org/COVID-19.
- 01:23:57 And I'm joined once again by Sri.
- 01:24:00 I know that you've been following social,
- 01:24:02 so tell us what has stood up for you so far.
- 01:24:05 [SRI SRIDHAR] Thanks, Juliette.
- 01:24:06 So today's Hashtag was #vaccines4all,
- 01:24:09 and we've gotten a lot of comments
- 01:24:10 from folks all over the world,
- 01:24:12 including the United States, Venezuela,
- 01:24:15 Saudi Arabia, Spain, Ethiopia, India,
- 01:24:18 Ireland, the Switzerland, Uganda
- 01:24:20 and also the United Kingdom.
- 01:24:22 But what have people been talking about online?
- 01:24:25 Quite a few things.
- 01:24:26 They have been talking about the importance
- 01:24:28 of making vaccines more available to everyone,
- 01:24:31 as well as raising awareness about their safety,
- 01:24:34 about ensuring the technology to produce vaccines is shared
- 01:24:38 and also the importance of pandemic preparedness
- 01:24:41 and also disease surveillance.
- 01:24:43 We've also been monitoring some comments across social media,
- 01:24:46 so I did want to give a shout out
- 01:24:48 to a couple of comments that have come out on LinkedIn.
- 01:24:51 We have a comment here from Alex Mutiso,
- 01:24:53 who says that we now have a cure for malaria,
- 01:24:56 but let's work together to fight not just COVID,
- 01:24:59 but also other social, environmental and health issues
- 01:25:02 that impact the poor disproportionately.
- 01:25:05 So I think a good reminder
- 01:25:06 about some of the other major health crisis
- 01:25:09 still in the world today.
- 01:25:10 And we also have a comment from a Atul Save,
- 01:25:13 who says currently we are facing
- 01:25:15 a shortage of COVID-19 vaccines.
- 01:25:17 Many people are unable to get vaccinated
- 01:25:20 due to inadequate supplies,
- 01:25:21 which is something you and I
- 01:25:23 were just talking about a bit earlier
- 01:25:25 about that being quite a crisis.
- 01:25:28 Yeah, it's absolutely heart-breaking.
- 01:25:29 And I know that we have the poll.
- 01:25:31 Do we finally have those results?
- 01:25:32 Yes, we do have the poll results.
- 01:25:34 Today's poll asked what is most important
- 01:25:36 to ensure equitable and successful
- 01:25:39 COVID-19 vaccine deployment.
- 01:25:41 Now, as a reminder, the four choices were
- 01:25:44 was it having an adequate stock of vaccines,
- 01:25:46 a sufficiently funded, resilient and inclusive health system,
- 01:25:50 enough equipment and trained public health personnel,
- 01:25:53 or D, engagement of local community leaders
- 01:25:56 and organizations?
- 01:25:57 So before we get to the big reveal, how did you vote?
- 01:26:00 [JULIETTE POWELL] Alright, so if I had my druthers,
- 01:26:02 I would have said E all of the above.
- 01:26:05 [SRI SRIDHAR] Okay, that's a choice.
- 01:26:06 I went for A, but shall we see how people voted?
- 01:26:10 Okay.
- 01:26:14 So 44.3% of the votes goes
- 01:26:16 to a sufficiently funded resilient
- 01:26:18 and inclusive health system,
- 01:26:20 followed by having an adequate stock of vaccines,
- 01:26:23 enough equipment and trained public health personnel,
- 01:26:26 and finally engagement
- 01:26:27 of local community leaders and organizations.
- 01:26:30 [JULIETTE POWELL] Thank you so much, Sri.
- 01:26:31 [SRI SRIDHAR] Thanks, Juliette.
- 01:26:34 [MAN] Hi. I'm [inaudible], in Khartoum, Sudan.
- 01:26:36 And you're watching the World Bank-IMF Annual Meetings.
- 01:26:45 [MAN] ¡Hola! I'm [inaudible] in Montelíbano, Colombia,
- 01:26:49 and you're watching the World Bank-IMF Annual Meetings.
- 01:26:55 [JULIETTE POWELL] Our audience has been posting questions
- 01:26:58 before and throughout this entire broadcast,
- 01:27:01 and now we are joined live by two World Bank Group experts
- 01:27:05 to respond to some of those questions.
- 01:27:08 We have with us Mamta Murthi,
- 01:27:10 who is the World Bank vice president
- 01:27:12 for Human Development,
- 01:27:13 and Stephanie Von Friedeberg,
- 01:27:15 who is the senior vice president of Operations at the IFC,
- 01:27:18 which is the private sector arm of the Bank.
- 01:27:21 And thank you both for joining us today.
- 01:27:23 We really appreciate it.
- 01:27:24 We're going to start out by the most popular question
- 01:27:28 that came to us from our Francophone audience,
- 01:27:31 in particular.
- 01:27:32 And this is coming from Ndege Mamy Valerie.
- 01:27:36 She's in the Democratic Republic of Congo
- 01:27:39 and she sent us a video.
- 01:27:41 [HI, MY NAME IS NDEGE MAMY VALERIE]
- 01:27:44 [FROM THE DEMOCRATIC REPUBLIC OF CONGO]
- 01:27:47 [IN THE PROVINCE OF EQUATEUR.]
- 01:27:49 [MORE PRECISELY IN THE CITY OF MBANDAKA.]
- 01:27:51 [MY QUESTION IS: HOW HAS THE WORLD BANK ORGANIZED ITSELF]
- 01:27:55 [SO THAT THE DEVELOPING COUNTRIES CAN OBTAIN]
- 01:27:58 [AFFORDABLE ANTI-COVID VACCINES?]
- 01:28:01 [THANK YOU.]
- 01:28:05 [JULIETTE POWELL] I'd love to pose the question
- 01:28:06 to both of you, starting with you, Mamta.
- 01:28:08 And just to recap the question in English,
- 01:28:12 can you tell us just a little bit more about how you feel
- 01:28:16 the World Bank has organized itself
- 01:28:18 so that developing countries
- 01:28:20 can really obtain affordable COVID vaccines.
- 01:28:24 [MAMTA MURTHI] Thank you, Juliette, for that question.
- 01:28:26 And also thank you for the question coming in from DRC,
- 01:28:29 a country that I'm hoping to visit in a couple of weeks time.
- 01:28:33 I would say that the World Bank Group has done four things.
- 01:28:37 First of all, it's made a financing envelope available,
- 01:28:41 a significantly large financing envelope available
- 01:28:45 so that countries can buy these vaccines
- 01:28:48 and deploy them in country.
- 01:28:50 So as of a week or so ago,
- 01:28:53 already $6 billion had been committed
- 01:28:56 from this envelope to support purchase and deployment
- 01:29:01 in over 60 countries in the world.
- 01:29:05 From that money,
- 01:29:06 countries have already contracted nearly
- 01:29:09 a quarter of a billion doses of COVID-19 vaccines,
- 01:29:14 and a hundred million of those doses
- 01:29:16 will be delivered this calendar year.
- 01:29:19 So there's a part which relates to just resources for purchase.
- 01:29:24 The second part relates to support for deployment,
- 01:29:28 because as we've heard it's not enough
- 01:29:30 to get the vaccines to the country.
- 01:29:32 They actually have to go into people's arms.
- 01:29:35 And a lot of the support that we're providing
- 01:29:38 with partners on the ground is to support deployment.
- 01:29:42 You had this video from Côte d'Ivoire earlier, right?
- 01:29:46 Côte d'Ivoire is one of the countries
- 01:29:48 where the World Bank is working,
- 01:29:50 and we've supported the government
- 01:29:51 and ramping up vaccinations.
- 01:29:55 And we've done this by helping community leaders
- 01:29:59 and social influencers talk about vaccines
- 01:30:02 and how they're safe and how they're effective.
- 01:30:05 We're also supporting mobile clinics
- 01:30:07 that can go out to markets, to small villages,
- 01:30:09 tell people about the vaccines and also vaccinate them.
- 01:30:12 The third thing we're doing
- 01:30:14 is supporting the manufacturer of vaccines and peripherals.
- 01:30:19 And I have my colleague Stephanie here,
- 01:30:21 who's going to say a lot more about it.
- 01:30:23 So let me move on to the fourth thing that we're doing.
- 01:30:25 We're doing a lot of advocacy
- 01:30:28 so that developing countries
- 01:30:29 can have their vaccine contracts fulfilled.
- 01:30:32 And you heard from the Multilateral Leaders Task Force
- 01:30:36 from David, Kristalina, Tedros and others
- 01:30:39 about how important this is.
- 01:30:40 Because most of the vaccines have been delivered
- 01:30:43 and are being delivered in the richest countries of the world.
- 01:30:47 And we're saying
- 01:30:48 that manufacturers need to now reprioritize
- 01:30:51 and make sure that the contracts that are in place are satisfied.
- 01:30:56 The developing country contracts
- 01:30:58 that are in place need to be satisfied.
- 01:31:00 [JULIETTE POWELL] Absolutely.
- 01:31:01 I don't think anybody would disagree with that.
- 01:31:03 Stephanie, would you also like to respond to the question?
- 01:31:05 [STEPHANIE VON FRIEDEBURG] Absolutely, Juliette.
- 01:31:07 It's a great question.
- 01:31:08 It's a good follow on to the conversation
- 01:31:10 Mamta and I had at the Spring Meetings.
- 01:31:12 At the start of the Pandemic,
- 01:31:14 and you said this, IFC is the private sector arm
- 01:31:16 of the World Bank,
- 01:31:17 we actually thought our job was to ensure
- 01:31:20 that companies stayed afloat
- 01:31:21 and that we maintained jobs in our countries of operation.
- 01:31:25 So we created this $8 billion facility
- 01:31:27 for our existing clients and thought this is our way forward.
- 01:31:30 But then we quickly realized
- 01:31:32 that this wasn't just an economic crisis.
- 01:31:34 It was a health crisis, and we needed to do more.
- 01:31:37 And we could see from our conversations
- 01:31:40 with producers, and for people in our countries of operation,
- 01:31:44 that most of the equipment and the supplies,
- 01:31:46 to say nothing of vaccines,
- 01:31:47 were all being produced and consumed in the developed world.
- 01:31:51 And we knew we needed to do something different.
- 01:31:53 So we went back to our board, and we sought approval
- 01:31:57 for a $6 billion global health platform.
- 01:32:00 The idea was to help the production of PPE, equipment,
- 01:32:04 pharmaceuticals in our countries of operation.
- 01:32:07 And imagine when we did that,
- 01:32:09 we tacked vaccines on literally the last day
- 01:32:11 before we went to the board as a just in case.
- 01:32:14 So I'm actually really pleased to say that as of today,
- 01:32:17 we've invested $1.9 billion across the globe
- 01:32:21 in companies like Fosun in China,
- 01:32:24 Bio-E, who we heard from in India earlier today.
- 01:32:27 Our flagship project was a €600 million project
- 01:32:31 that we did with a group of DFIs
- 01:32:34 to produce 300 million doses of the Johnson & Johnson vaccine
- 01:32:39 on the continent of Africa
- 01:32:41 with a company called Aspen Pharmaceuticals.
- 01:32:43 But we know that that's not enough,
- 01:32:45 and we need to continue to push the envelope.
- 01:32:48 So we have created a new initiative with CEPI to help us.
- 01:32:52 We're partnering
- 01:32:53 with the Institut Pasteur in Dakar, Senegal,
- 01:32:56 to see if we can actually build an mRNA facility for later use.
- 01:33:00 And we're working very closely
- 01:33:02 with the government of Rwanda
- 01:33:04 to create an entire ecosystem to think through
- 01:33:07 how do you actually create
- 01:33:08 pharmaceuticals and vaccines on a more holistic basis?
- 01:33:12 It's a really heavy lift, but it's critical for us
- 01:33:15 as we move forward and come out of the crisis
- 01:33:18 to ensure that when the next pandemic hits,
- 01:33:20 our countries are better prepared.
- 01:33:22 [JULIETTE POWELL] I couldn't agree with you more.
- 01:33:24 And I'm glad to hear you talking
- 01:33:26 about assuring up the entire ecosystem.
- 01:33:28 I think that's absolutely fundamental.
- 01:33:30 We've got our second question for you,
- 01:33:33 and this is coming in
- 01:33:35 from [inaudible], he's in India.
- 01:33:38 And he asked:
- 01:33:40 can you predict the next era of COVID or pandemic?
- 01:33:46 [MAMTA MURTHI] That's a great question.
- 01:33:48 The answer to that is no one can predict
- 01:33:52 what the next pandemic will be or even when.
- 01:33:57 But what we can say with certainty
- 01:33:59 is there will be another pandemic.
- 01:34:01 Without a doubt.
- 01:34:02 We know, at least in the past 50 years or so
- 01:34:05 that most of these pandemics have arisen
- 01:34:08 because of the contact between humans and animals.
- 01:34:11 That's why they're called zoonotic.
- 01:34:14 And with urbanization, with intensive agriculture,
- 01:34:17 with what's happening globally,
- 01:34:19 we can expect another pandemic to emerge
- 01:34:22 because of this interaction between humans and animals.
- 01:34:27 We are saying that countries need to be prepared,
- 01:34:30 no matter when this arises, because it will arise.
- 01:34:34 And we really see four things as being important
- 01:34:38 for the next pandemic.
- 01:34:41 To fight it, countries need strong health systems.
- 01:34:44 We've learned from this pandemic
- 01:34:46 that if you don't have a strong core primary health care system,
- 01:34:49 you're not going to be able to detect
- 01:34:51 or treat or respond to the pandemic.
- 01:34:54 And so as the World Bank,
- 01:34:56 we're placing a lot of emphasis
- 01:34:57 on building strong health systems.
- 01:34:59 The second thing we've learned
- 01:35:01 is that you need regional and global cooperation.
- 01:35:05 I mean, a pandemic does not stop at the border.
- 01:35:08 It doesn't need a passport
- 01:35:09 to go from one part of the world to another.
- 01:35:11 And so we've also supported regional monitoring
- 01:35:15 and surveillance systems.
- 01:35:16 In Western Central Africa,
- 01:35:18 we have a great project which is called REDISSE,
- 01:35:21 and it's actually supported networked surveillance
- 01:35:24 and monitoring systems
- 01:35:26 to detect and respond to emerging diseases.
- 01:35:29 We've also supported the Africa Center for Disease Control,
- 01:35:33 which has been playing a fantastic role in this pandemic.
- 01:35:37 It's not just regional cooperation.
- 01:35:39 One needs to think of multisector responses.
- 01:35:42 Think of this pandemic.
- 01:35:43 One of the ways of responding to it
- 01:35:46 was asking people to stay at home
- 01:35:48 so that it would not spread.
- 01:35:50 But if you ask people to stay at home,
- 01:35:51 how are they going to earn an income?
- 01:35:53 And that's why having some sort
- 01:35:55 of cash benefit or transfer was very important.
- 01:35:58 Both for households, but also for small businesses.
- 01:36:02 A multi sector and a multicountry response
- 01:36:05 is the second thing we've learned is necessary.
- 01:36:08 The third thing we've learned is distributed manufacturing.
- 01:36:12 That's the key to having some kind of global health security.
- 01:36:15 And I think IFC and others
- 01:36:17 play an incredibly important role here.
- 01:36:19 And I think the final thing that we've learned
- 01:36:22 is that you really need to fund these things adequately.
- 01:36:26 We heard Ngozi talk this morning earlier today
- 01:36:29 about how countries need to spend much more themselves.
- 01:36:32 Right.
- 01:36:33 She talked about a 1% increase in GDP spending
- 01:36:37 to support pandemic preparedness.
- 01:36:40 And she also talked about better network global architecture.
- 01:36:44 So we need all of these things
- 01:36:46 so that we can prepare for the next pandemic,
- 01:36:49 even though we don't know exactly what it's going to be.
- 01:36:53 [JULIETTE POWELL] I feel like you've, in part,
- 01:36:54 answered our final question today.
- 01:36:57 This was the most popular question
- 01:36:59 that was sent in by the audience that's watching.
- 01:37:02 They really want to know the answer to this question,
- 01:37:06 which is what kind of transformation is needed
- 01:37:09 for health care systems in poor countries?
- 01:37:11 In other words,
- 01:37:12 how do we make the health systems more resilient
- 01:37:16 now and in the future?
- 01:37:19 How does that work?
- 01:37:21 [MAMTA MURTHI] I would say they have to be stronger.
- 01:37:24 They have to be better resourced with trained personnel
- 01:37:29 with the ability to surge, right?
- 01:37:32 Suppose you have the emergence of a disease,
- 01:37:34 you need more people working on it.
- 01:37:36 You need the ability to detect and prevent disease.
- 01:37:42 And that means you really have to take a one health approach.
- 01:37:45 You've got to look not just at human disease,
- 01:37:48 but you've got to look at animal disease
- 01:37:50 and how these two are interacting.
- 01:37:53 And then I think you need
- 01:37:54 strong regional and global institutions.
- 01:37:57 I like very much what Kristalina said
- 01:38:00 at the end of the leader segment
- 01:38:02 where she said, what this pandemic has done is
- 01:38:05 it's shown that if you have a weak immune system,
- 01:38:08 you're going to fall sick.
- 01:38:10 It's the same with countries.
- 01:38:11 If you don't have a resilient health system
- 01:38:14 or a means of dealing with an emergency,
- 01:38:16 you're not going to be able to deal with a pandemic.
- 01:38:19 So I think institutional development,
- 01:38:21 starting with strong health systems,
- 01:38:23 is probably what's needed.
- 01:38:24 [JULIETTE POWELL] Stephanie, did you have a thought
- 01:38:26 really briefly before we go on?
- 01:38:28 [STEPHANIE VON FRIEDEBURG] So I actually do.
- 01:38:31 When I look at the conversation we've had,
- 01:38:34 we've been talking a lot about shots and arms,
- 01:38:36 which was a critical imperative for us in the short term.
- 01:38:40 But we need to redouble our efforts
- 01:38:42 to build a more holistic system around the world
- 01:38:45 and at the country level.
- 01:38:47 And that really starts with thinking
- 01:38:49 about things like how do we get modern equipment
- 01:38:52 into places like Africa?
- 01:38:54 So one of the things that we've been working on
- 01:38:57 is a $300 million African medical equipment facility.
- 01:39:00 What it's designed to do...
- 01:39:02 We've partnered with GE and Philips and others,
- 01:39:05 and we're giving equipment through leases
- 01:39:08 and through acquisition to small clinics in Africa,
- 01:39:11 using financial institutions as intermediaries.
- 01:39:15 And why are we doing this?
- 01:39:16 So if you look at Africa,
- 01:39:18 WHO did a recent study that said
- 01:39:20 that only 11% of the countries in Africa
- 01:39:24 have one MRI machine for 1 million people,
- 01:39:28 and 24% for CT scans.
- 01:39:30 If you compare that to Europe,
- 01:39:33 countries in Europe have 89% better statistics on MRI
- 01:39:39 and 97% better statistics on CT scanners.
- 01:39:43 So we know we need to solve the fragmentation in Africa.
- 01:39:47 And working with GE and Phillips,
- 01:39:49 we can do that and bring the right technical skills.
- 01:39:51 I think the other thing that Mamta didn't mention,
- 01:39:54 which we've seen very repeatedly
- 01:39:56 is the need for public-private partnership.
- 01:39:59 So we've learned in our other countries of operation
- 01:40:01 that you can do this through public-private partnerships.
- 01:40:05 We've done really interesting work
- 01:40:06 in Turkey with hospitals,
- 01:40:08 and in Uzbekistan recently with dialysis clinics.
- 01:40:11 The other thing is we really need
- 01:40:13 to double down and focus on education.
- 01:40:15 And I think this is an area
- 01:40:17 where the Bank and IFC can really work together.
- 01:40:19 We need health technicians,
- 01:40:21 we need nurses and we need doctors at scale
- 01:40:23 to really make this work.
- 01:40:25 [JULIETTE POWELL] I couldn't agree with you more.
- 01:40:27 Thank you both for joining us,
- 01:40:29 and thank you for working together.
- 01:40:32 and to you, our viewers,
- 01:40:34 please do continue to post those questions.
- 01:40:36 We've got experts here
- 01:40:37 that are going to stay online
- 01:40:38 and they're really going to do their best
- 01:40:41 to answer all of them for you.
- 01:40:43 Young people have been deeply impacted by this pandemic
- 01:40:47 with the closing of schools.
- 01:40:49 You've got separation from friends and from family.
- 01:40:51 They're all struggling to cope,
- 01:40:53 and they worry about being left behind, and with good reason.
- 01:40:56 But they're also incredibly optimistic about their futures.
- 01:41:00 So we asked some young people from around the world
- 01:41:03 to talk about what it was
- 01:41:04 that the vaccine means for them and their communities,
- 01:41:08 and what they can really look forward to doing
- 01:41:10 once they're vaccinated.
- 01:41:15 [RADHIKA BATRA] COVID has devastated us all
- 01:41:17 due to loss of lives,
- 01:41:18 financial loss, loss of jobs.
- 01:41:21 [COVID-19 HAS BROUGHT A NEGATIVE IMPACT ON MY LIFE OVERALL.]
- 01:41:24 [IT'S DEFINITELY SOMETHING THAT I, AN ALL OF US,]
- 01:41:28 [DID NOT EXPECT.]
- 01:41:29 [SEDIGHE KARIMZADEH] Currently we lack basic sanitation
- 01:41:32 and health services.
- 01:41:33 We are at greatest risk of transmission.
- 01:41:36 [FANNY BESSEM] Because many of the results
- 01:41:38 that we are available have been diverted to COVID.
- 01:41:42 It's very challenging,
- 01:41:44 and the mental health issues are just tremendous.
- 01:41:47 [LAVAU NALU] I haven't seen a lot of my family
- 01:41:49 and a lot of my friends for so long
- 01:41:51 and I can't wait for that day when we're all here together.
- 01:41:54 [MIRIAM LIVRAMENTO] I believe in science,
- 01:41:55 I believe in immunization
- 01:41:57 through vaccination.
- 01:41:58 [YANA PANFILOVA] On behalf young people,
- 01:42:00 the most important thing:
- 01:42:01 the vaccine gives us assurance that we will not be locked down.
- 01:42:07 We will not again feel the weight of this pandemic
- 01:42:11 on our shoulders.
- 01:42:13 [PATELISIO PATELISIO] Getting vaccinated means
- 01:42:14 I get to protect myself
- 01:42:16 and my family.
- 01:42:17 [MIRIAM LIVRAMENTO] It means we can have these streets
- 01:42:20 full of turists again.
- 01:42:22 And we can have opportunities for young people like me
- 01:42:25 to grow our business.
- 01:42:27 [MAMELLO MAKHELE] Once I get vaccinated against COVID-19,
- 01:42:30 I'll be able to socially interact with my friends
- 01:42:33 without fear of being sick.
- 01:42:35 [LAVAU NALU] Being vaccinated means
- 01:42:37 that my family can be reconnected here,
- 01:42:39 in Papua New Guinea [inaudible].
- 01:42:41 [RADHIKA BATRA] We will live without the fear
- 01:42:42 of losing a loved one.
- 01:42:43 There will be jobs and food on the table.
- 01:42:46 [EMMANUELE MARIE PARRA] I can attend and hear
- 01:42:48 live masses in Church with family.
- 01:42:50 [FANNY BESSEM] Our lives can go back to normal.
- 01:42:52 We can go to markets.
- 01:42:53 We can attend our family meetings.
- 01:42:55 We can go to the communities and work without fear.
- 01:42:58 [CARLOS MADRIGAL IBERRI] We can go back to the streets
- 01:43:00 with the patients,
- 01:43:02 so we can get to transform the hearts
- 01:43:04 of the population in Mexico.
- 01:43:06 [SEDIGHE KARIMZADEH] So getting vaccinated would mean
- 01:43:09 we can still take one more step to save our lives.
- 01:43:12 -[PATELISIO PATELISIO] We want... -[MAMELLO MAKHELE] ...to get vaccinated...
- 01:43:14 - [YANA PANFILOVA] ...so life... - [SEDIGHE KARIMZADEH] ...can return
- 01:43:15 [CARLOS MADRIGAL IBERRI] ...to normal.
- 01:43:22 And this brings us to the end of this event.
- 01:43:25 I really want to thank our guests for joining us
- 01:43:27 and sharing an incredibly important discussion.
- 01:43:30 Of course, I want to thank you, our viewers.
- 01:43:32 We've still got much more to come
- 01:43:34 for these Annual Meetings on Thursday.
- 01:43:36 We're going to be discussing
- 01:43:38 how we can make climate action count
- 01:43:40 and then to round off the week,
- 01:43:42 we're going to be focusing
- 01:43:43 on the role of trade in supporting economic growth.
- 01:43:46 Of course, you can watch all of those
- 01:43:48 as well as replay of this event at live.WorldBank.org.
- 01:43:52 And of course,
- 01:43:53 we hope that you've all enjoyed hearing
- 01:43:55 from our distinguished guests at today's event.
- 01:43:58 And do continue sharing all of those comments,
- 01:44:01 we'd absolutely love to hear from you again.
- 01:44:03 My name is Juliette Powell,
- 01:44:04 and thank you so much for joining us today!
Ending the Pandemic: The Road to an Inclusive Recovery
The World Bank convened global and regional leaders, along with representatives of the private sector, civil society, and youth to make a powerful case for more equitable access to vaccines for developing countries and emphasize the importance of strong health systems to successful vaccine deployment and better pandemic preparedness.
Heads of organizations leading the Task Force on COVID-19 Vaccines, Therapeutics and Diagnostics for Developing Countries shared their perspectives on ending the pandemic and building a truly inclusive recovery.
Mother and daughter in the Philippines talked about their experience with the pandemic, and we learned how the World Bank’s support has impacted the health systems and people in Cote d’Ivoire.
International Finance Corporation’s Managing Director led a conversation on the critical role the private sector plays in fighting the pandemic.
We heard from the Deputy Director of Africa CDC on the need for regional collaboration to combat the pandemic.
Civil society leaders shared what their organizations are doing to tackle the pandemic and what actions they expect from international organizations.
Finally, World Bank Group experts answered questions from the audience.
The event concluded with reflections from young people from around the world on what the vaccine means for them and their communities and what they look forward to doing once vaccinated.
Event Program
Moderated, dynamic discussion with the heads of organizations leading the Task Force on COVID-19 Vaccines, Therapeutics and Diagnostics for Developing Countries.
- David Malpass, President, WBG
- Kristalina Georgieva, Managing Director, IMF
- Tedros Adhanom Ghebreyesus, Director General, WHO
- Ngozi Okonjo-Iweala, Director General, WTO
- Moderated by: Becky Anderson, CNN International
Conversation with private sector leaders on the key role of private sector in playing on vaccines for developing countries through the production and manufacturing of therapeutics, testing and vaccines essential for halting the spread.
- Narender Mantena, Head of Global Strategy, Biological E. Limited / CEO, BE Pharmaceuticals Inc.
- Strive Masiyiwa, African Union Special Envoy and coordinator of the Africa Vaccine Acquisition Task Team (AVATT)
- Moderator: Makhtar Diop, MD IFC
- Dr. Ahmed Ogwell Ouma, Deputy Director of Africa CDC
- Moderated by: Juliette Powell, Media Commentator
- Mamta Murthi, Vice President Human Development, World Bank
- Stephanie von Friedeburg, Senior Vice President, Operations, IFC
- Moderated by: Juliette Powell, Media Commentator
Voices from civil society and youth.
- Nadia Daar, Oxfam, Washington DC
- Priscilla Nyaaba, Youth Harvest Foundation Ghana
- Youth: Including Friends from One Young World
Polls & Questions From the Audience
? What is most important to ensure equitable and successful COVID-19 vaccine deployment? Four options and thousands of votes! Check out the results of the #Vaccines4All poll. Learn more by watching the replays of the 2021 WBG-IMF Virtual Annual Meetings: https://t.co/YZRLoq86tO pic.twitter.com/kUR5pJxrR4
— World Bank Live (@WorldBankLive) October 13, 2021
72 VOTES / Anonymous
How are international organizations helping poor countries obtain and distribute COVID vaccines?
59 VOTES / Anonymous
How do we achieve inclusive recovery after the COVID pandemic?
38 VOTES / Gladys
How can we confront misinformation about vaccines to protect life and global public health?
30 VOTES / Anon
You talk about transformations needed for health care systems in poor countries. What kind of transformations are needed?
26 VOTES / Kadigia Ali Mohamud
How do we vaccinate Africa's population if we do not have the exact information for the resident population in a territory?
Resources
Read the transcript
- 00:00 [Upbeat Music]
- 00:02 [Annual Meetings 2021]
- 00:14 [COMING UP] [ENDING THE PANDEMIC: THE ROAD TO AN INCLUSIVE RECOVERY]
- 00:22 Hello and welcome to Ending the Pandemic,
- 00:26 The Road to an Inclusive Recovery.
- 00:29 I'm Becky Addison live from CNN's Broadcasting Hub
- 00:32 here in Abu Dhabi in the UAE,
- 00:35 [BECKY ANDERSON, CNN PRESENTER] bringing you this special event
- 00:37 alongside the 2021 World Bank-IMF Annual Meetings.
- 00:42 Today, we've reached a critical moment.
- 00:45 We can either take urgent action to end the pandemic
- 00:49 and get the global economy back on track, or
- 00:52 we must reconcile ourselves with the world
- 00:54 where the pandemic will ebb and flow
- 00:56 and where our economies will never reach their true potential.
- 01:01 Here's the deal.
- 01:02 If we want to move beyond this pandemic,
- 01:06 we must make sure at least 40% of all people, in all countries,
- 01:12 are vaccinated by the end of this year.
- 01:16 That is the message from the leaders
- 01:19 I have joining me here today.
- 01:20 They have come together establishing a task force
- 01:24 aimed at doing just that.
- 01:27 I'm delighted to be joined from Washington
- 01:30 by the World Bank President David Malpass,
- 01:34 IMF Chief Kristalina Georgieva,
- 01:39 the WTO Director-General Ngozi Okonjo-Iweala,
- 01:45 and from Geneva, the WHO Director-General
- 01:49 Tedros Adhanom Ghebreyesus.
- 01:54 Choices we make in the coming years will determine
- 01:57 whether developing countries suffer a lost decade
- 02:00 or can usher in rapid growth and economic transformation.
- 02:04 Those are the worlds of the World Bank head, David Malpass.
- 02:08 Bottom line, we can't recover without global cooperation and coordination.
- 02:12 We can't get there without tackling vaccine inequality.
- 02:16 According to the Global Dashboard for Vaccine Equity,
- 02:20 established in part by the WHO as of October 6th,
- 02:24 61% of those living in high income countries
- 02:28 have been jabbed with at least one shot.
- 02:32 That figure drops to less than 4% in low-income countries.
- 02:38 Less than 4%.
- 02:41 Let that sink in.
- 02:44 The goal of the Multilateral Leaders Task Force
- 02:47 is to figure out essentially how to close this gap.
- 02:50 To suggest that there is an alarming shortage of supply
- 02:54 is to, frankly, understate the extent of the problem.
- 02:58 So, David, I'd like to start with you this evening.
- 03:01 What is needed to boost vaccine supply and access
- 03:06 in developing countries?
- 03:07 Let's start there.
- 03:10 [DAVID MALPASS] Thanks, Becky. And you're right.
- 03:12 [DAVID MALPASS, PRESIDENT, WORLD BANK GROUP] 40% is the goal
- 03:14 and that's not being achieved.
- 03:16 What we need to do, and it's particularly apparent in Africa
- 03:20 is to get doses to people that are ready to deliver them.
- 03:23 There is plentiful supply.
- 03:26 The production is going up very rapidly
- 03:29 in the advanced economies.
- 03:31 But there's a gap between the donations
- 03:33 and the actual deliveries of those donated doses
- 03:36 in particular Africa.
- 03:39 What we need to do is get the donators,
- 03:44 the countries that have excess vaccines to state and follow through
- 03:48 in an accountable way with the deliveries,
- 03:52 the dates of the delivery, the type of the vaccine
- 03:55 that's going into the developing countries.
- 03:58 World Bank can help in a number of areas.
- 04:01 We have financing available.
- 04:02 We right now have AVAT, a contract within Africa
- 04:06 that's been successful in getting doses to people
- 04:09 We have today 250,000 doses under contract
- 04:14 that will be delivered.
- 04:15 So we're trying to have early delivery dates
- 04:18 for the donations that have been committed
- 04:21 by the advanced economies.
- 04:23 We need to know what type of vaccine is
- 04:27 and where it's going to be delivered
- 04:29 so we can work on the hesitancy problem.
- 04:32 [BECKY ANDERSON] Right. Okay.
- 04:33 Tedros, you and I have been talking
- 04:36 vaccine inequality for over twelve months.
- 04:38 Progress, with respect to all of you, has been painfully slow.
- 04:44 I know, you know that.
- 04:46 Firstly, are these donations enough, sir?
- 04:54 [TEDROS ADHANOM GHEBREYESUS] Yeah. Thank you, Becky.
- 04:56 The donations are not enough.
- 04:58 And to be honest, as you said, very slow.
- 05:01 [DR. TEDROS ADHANOM GHEBREYESUS, DIRECTOR-GENERAL, WHO] Plus,
- 05:04 it's very disappointing that it's taking so long
- 05:08 for the world to really commit.
- 05:11 Epidemiologically, it's wrong
- 05:13 because we cannot end this pandemic.
- 05:15 Economically, it's wrong because the economy globally is not recovering
- 05:21 and it is also morally wrong.
- 05:26 There should be a political commitment to address this problem.
- 05:30 As you have rightly said, if you take low-income countries,
- 05:33 it's only 4%, and if you take it in another way
- 05:37 70% of the deliveries are done just to 10 countries,
- 05:42 That's completely unfair.
- 05:47 This will not end the pandemic.
- 05:49 It's in the interest of all countries
- 05:52 rich, poor or middle-income to end this pandemic.
- 05:57 And that's why, together with my colleagues in the task force,
- 06:01 we are saying there is a 40% by the end of this year target,
- 06:06 and 70% by the mid of next year.
- 06:09 We have to, especially when G20 countries should own those targets
- 06:14 and make it happen
- 06:15 because more than 80% of the economy belongs to them.
- 06:20 The bulk of the production capacity also belongs to them.
- 06:24 If there is political commitment and they want to do it, they can do it.
- 06:28 So that's what we're asking.
- 06:30 [BECKY ANDERSON] That's a big question, though, isn't it?
- 06:32 That's the big question.
- 06:33 Is the political commitment on standby?
- 06:35 I just want to bring other two gets in tonight.
- 06:38 Let's be quite clear about this.
- 06:40 Ngozi, let me start with you.
- 06:42 Just how realistic are these targets at this point?
- 06:46 We are talking at least 40% of people in every country vaccinated
- 06:50 by the end of 2021 and at least 60% by mid 2022.
- 06:56 We are way away from those levels at this point.
- 07:02 [NGOZI OKONJO-IWEALA] Well, thank you very much, Becky.
- 07:05 I think that with these targets,
- 07:07 we are well aware you can see the numbers
- 07:10 [NGOZI OKONJO-IWEALA, DIRECTOR-GENERAL, WTO] that you talked about
- 07:12 4% in low-income countries, 60% in rich countries.
- 07:19 But if you can see the progress that can be made in countries
- 07:23 when they have access to these vaccines
- 07:25 and where the ability to distribute them
- 07:28 and get them into arms there.
- 07:31 So I think if we decide as a community
- 07:35 that we can do this, we will do it.
- 07:37 We are very far away from where we need to be.
- 07:40 But we need to ramp up now
- 07:42 because as Tedros said, it's just not acceptable
- 07:45 that we have this gap.
- 07:47 So let's get the vaccines delivered quickly.
- 07:50 We have countries waiting to put these vaccines into arms.
- 07:55 Let's get them delivered and we may be able
- 07:57 to achieve this target.
- 07:59 This might be ambitious, given where we are now.
- 08:01 But it's not impossible.
- 08:03 [BECKY ANDERSON] Kristalina standby because I do want to get
- 08:06 your perspective on this.
- 08:08 The cold, hard fact, according to Amnesty International,
- 08:13 out of the nearly 6 billion COVID-19 doses delivered worldwide,
- 08:18 a poultry 0.3% have gone to low-income countries.
- 08:23 And at this point I just want to draw on some CNN reporting
- 08:28 to underscore the challenge here.
- 08:30 Let's look at Africa, for example, standby.
- 08:42 [JOHANNESBURG] [SOUTH AFRICA]
- 08:43 [Dave McKenzie] I'm Dave McKenzie in Johannesburg.
- 08:44 If you look around me, life seems to be getting back to normal.
- 08:48 But this country, in this region,
- 08:50 has suffered through a devastating COVID-19 pandemic.
- 08:53 The big issue now, to avoid future waves,
- 08:56 is of course, vaccines.
- 08:58 Vaccine nationalism and vaccine hoarding
- 09:01 has really hit the efforts for an equitable access
- 09:04 across the world, particularly in Africa,
- 09:07 for COVID-19 vaccines.
- 09:08 In the African continent,
- 09:09 there are far less than 10% of people
- 09:12 who've received their full complement of COVID-19 vaccines,
- 09:17 Even as rich countries are giving booster shots
- 09:20 to the most vulnerable.
- 09:22 Now, the issue is,
- 09:23 as manufacturers ramp up vaccination production,
- 09:28 can the money and the resources be made available
- 09:30 to get vaccines optimations on the African continent,
- 09:34 or can there be a deal made
- 09:36 on dropping intellectual property of those vaccines?
- 09:40 All I can say is
- 09:41 through all my reporting on this issue
- 09:43 is the talk of solidarity has largely been talk.
- 09:48 Now it's time for action.
- 09:50 [BECKY ANDERSON] Kristalina, get the money and resources
- 09:52 to where they matter most is David's appeal.
- 09:56 What is being done to address finance and trade barriers
- 10:01 to ensure that vulnerable populations get these life saving tools?
- 10:08 [KRISTALINA GEORGIEVA] Thank you very much for bringing us together, Becky.
- 10:11 What we have seen is
- 10:13 [KRISTALINA GEORGIEVA, MANAGING DIRECTOR, IMF]
- 10:14 much more awareness
- 10:16 of the economic significance of overcoming
- 10:20 this great vaccination divide
- 10:24 and that awareness is slowly translating into
- 10:29 more willingness to act.
- 10:31 So, what do we know?
- 10:34 We know that the world economy is recovering,
- 10:37 that risks are going up
- 10:41 and the divergence in economic fortunes is expanding.
- 10:47 Why would that matters to advanced economies, to rich countries?
- 10:52 Because if the world continues to be slow to recover,
- 10:59 held back a lot by access to vaccines
- 11:03 by limited fiscal space,
- 11:05 that not only causes supply disruptions,
- 11:09 and the supply disruptions are one of the factors
- 11:13 pushing prices up.
- 11:16 But it also creates space for new variants of COVID
- 11:24 to flourish and run around the world.
- 11:26 We have done very careful analysis
- 11:30 that says that for $50 billion dollars,
- 11:35 we can achieve the target of vaccinating 40%
- 11:41 by the end of this year.
- 11:44 70%, actually Tedros lifted up to 70% target by mid 2022.
- 11:53 Of this 50 billion,
- 11:55 we now see close to two thirds being made available.
- 12:02 But we still have a gap to feel.
- 12:06 What are we doing?
- 12:08 I want to praise the World Bank for stepping up.
- 12:12 They are now willing and able to secure 20 billion in financing.
- 12:18 We, the IMF, have provided the largest in our history allocation
- 12:24 of the so called special drawing rights to
- 12:28 reserve assets of the IMF that gives countries fiscal space.
- 12:33 Where are the bottlenecks?
- 12:37 I do strongly believe there are two.
- 12:40 One, it is timely, allocation of vaccines
- 12:46 to developing countries.
- 12:48 If a rich country doesn't need the vaccines in November,
- 12:52 they can receive them in February.
- 12:58 Move the delivery in November to the developing quote.
- 13:03 And secondly, and this is where
- 13:06 it is so important we work together,
- 13:10 getting a vail of vaccine to turn into a shot in the arm.
- 13:16 And in many poor countries,
- 13:18 it is this getting the vaccine from the town where it is stored
- 13:25 to the child or the woman or the man in a village up in the mountains
- 13:31 that is the toughest part of this delivery.
- 13:35 I want to answer your question honestly,
- 13:38 can we get to 40% everywhere?
- 13:40 This is going to be tough.
- 13:42 But can we get much closer to 40% everywhere?
- 13:47 And at more than 40% in many countries?
- 13:51 Yes, the vaccines are produced.
- 13:54 We have to make sure they get
- 13:56 where they would make a difference.
- 13:58 [BECKY ANDERSON] Would a decision by the developed world
- 14:03 to advise booster shots to its populations
- 14:10 prevent you as they task force from achieving your goal?
- 14:15 David.
- 14:16 [DAVID MALPASS] I don't think that's the key issue.
- 14:19 The production is going up so rapidly.
- 14:21 There may be enough to do boosters
- 14:23 and to reach targets in 2022.
- 14:28 The key thing that I would emphasize is
- 14:30 for finance ministers in countries and their health ministers
- 14:34 to seek contracts, to try to get delivery dates that are early
- 14:38 and to ask for them and to request them
- 14:41 and then for the advanced economies
- 14:44 to go along with that to help get the delivery dates.
- 14:48 I was in Sudan.
- 14:50 Well, let me mention two things.
- 14:52 J&J doses are particularly valuable in Africa.
- 14:55 Europe has committed to shipping J&J doses to Africa.
- 15:00 Complete that so the people can have those doses.
- 15:04 I was in Khartoum and then Amman last week.
- 15:07 They're vaccinating people day by day.
- 15:11 The hesitancy is going down as once people have vaccines
- 15:15 and if they have the syringes and the needles
- 15:18 that can be brought in with the shipments of the doses,
- 15:23 then the people are being vaccinated so that part of the system is working.
- 15:28 But we need more clear delivery dates from the various sources.
- 15:32 World bank has 61 countries that have programs with us
- 15:36 and we can expand that into 100 countries.
- 15:40 If the countries ask for doses
- 15:43 and arrange for getting the contract set up
- 15:46 in accountable way, that's key.
- 15:49 [BECKY ANDERSON] Tedros, I have to get your perspective
- 15:54 at this point on boosters?
- 15:58 [TEDROS ADHANOM GHEBREYESUS] Thank you, Becky.
- 16:00 On Boosters, I would go back to the figures
- 16:04 because the world should understand the inequity the injustice.
- 16:09 As I said earlier, 66.5 billion dollars have already been ministered.
- 16:16 Of this, Africa got only 166 million.
- 16:23 166 million for 1.2 billion people,
- 16:27 and the rest 6.3 billion is for the rest of the world.
- 16:31 Then I can show you in a different way.
- 16:34 For instance, if you take South America, North America,
- 16:36 Europe, Asia, China as a region,
- 16:40 all of them are above 50% at least with a single dose,
- 16:43 while Africa is only 7% single dosed or 4.8%.
- 16:49 So as a region, the focus should be that.
- 16:51 Bringing it back to boosters,
- 16:54 when there is only 166 million delivered in Africa for 1.2 billion,
- 17:01 to start with the booster is really the worst we could do
- 17:07 as a global community.
- 17:10 It's unjust and also unfair
- 17:14 because we will not stop this pandemic
- 17:17 by ignoring the whole continent
- 17:20 and the continent which doesn't have any manufacturing capacity or other means.
- 17:25 The world should come back to its senses.
- 17:27 I don't want to spread it by saying all low-income countries,
- 17:31 the concentration of the problem is in one continent.
- 17:35 Let's take that first. So on.
- 17:36 For boosters, for countries to move into boosters
- 17:40 without even providing single doses in Africa,
- 17:43 it is not right.
- 17:45 It has to be stopped
- 17:46 and countries should respect the moratorium.
- 17:49 Of course there are exceptions.
- 17:51 We can use it in immunocompromised populations.
- 17:55 Immunocompromised.
- 17:57 The rest is immoral, unfair, unjust and it has to stand.
- 18:02 [BECKY ANDERSON] Ngozi and Christine, I must get your perspective on this.
- 18:05 Ngozi, briefly.
- 18:08 [NGOZI OKONJO-IWEALA] Briefly, I think one of the ways
- 18:10 to solve this inequity of access,
- 18:12 which I agree totally with Tedros is unacceptable,
- 18:16 is to decentralize production.
- 18:19 If we are going to continue needing boosters
- 18:22 and things like that,
- 18:23 it's evident that we need to decentralize production
- 18:26 to some of the countries that have no capacity.
- 18:29 On the African continent,
- 18:31 there is 17% of the world population
- 18:33 and 0.2% of the manufacturing capacity.
- 18:36 We cannot continue importing 99% of our vaccines
- 18:41 At the WTO, we've actually been working
- 18:44 with manufacturers of these vaccines
- 18:46 to try and help them with their supply chain problems,
- 18:50 monitoring where they are bottled neck
- 18:52 so that they can be able to increase production,
- 18:55 and at the same time, working with them
- 18:57 to encourage them to set up of manufacturing
- 19:00 in emerging markets in developing countries.
- 19:03 And I think, Becky, that is yielding some fruit.
- 19:06 We've now had an announcement by Pfizer
- 19:09 of investment in South Africa and Aspen.
- 19:12 We've heard of Moderna is just saying that
- 19:16 it's going to set up some production facilities on the continent.
- 19:20 But we need to get the capacity to produce.
- 19:25 [BECKY ANDERSON] The three leading vaccine manufacturers,
- 19:28 BioNTech, Moderna and Pfizer could net $130 billion dollars
- 19:32 by the end of this year.
- 19:33 Ngozi, you're right,
- 19:34 We have seen some progress
- 19:36 in manufacturing plants being set up,
- 19:39 but are these manufacturers prolonging this pandemic
- 19:42 by putting profits before people?
- 19:47 [NGOZI OKONJO-IWEALA] We hear a lot about profits before people,
- 19:52 and obviously, if you look at their numbers,
- 19:54 it is true they're earning far more than they ever have.
- 19:59 So that's why we are working with them to say,
- 20:02 "the perception of this profit before the lives of people
- 20:08 is neither good publicly for you, nor for anyone.
- 20:13 So we're working with them to really try to get
- 20:16 partnerships on the continent,
- 20:19 in Latin America as well, in low-income countries,
- 20:22 so that they can demonstrate that for them
- 20:26 it's not profit, but it's people.
- 20:29 It's coming along.
- 20:30 I think we need the manufacturers
- 20:33 because without them, we're not going to be able
- 20:35 to manufacture vaccines, vaccines are complicated.
- 20:38 You need the technology transfer,
- 20:40 the know-how to be able to do it
- 20:43 along with the issues of intellectual property.
- 20:46 So we cannot alienate them but we have to persuade them
- 20:50 that it's better for them to be public citizens
- 20:53 and put people before profit.
- 20:57 [BECKY ANDERSON] Kristalina, I promised I'll come back to you.
- 20:59 I want to get your perspective on the idea that developing world
- 21:03 will go ahead and provide booster shots
- 21:05 when the developing world is in such dire need.
- 21:09 It has been a year since South Africa and India
- 21:12 first call for the suspension of intellectual property protection
- 21:15 on vaccines and related technologies.
- 21:18 This is something Ngozi has just been alluding to.
- 21:20 The UK, Norway, Switzerland and the EU
- 21:23 are still blocking waiver needed to make that happen.
- 21:28 Do you and do your fellow leaders here today
- 21:32 call on countries to back this proposal,
- 21:35 at least until the fight against the pandemic is over.
- 21:40 [KRISTALINA GEORGIEVA] We at IMF actually researched
- 21:42 the question of production versus availability,
- 21:48 and the answer is
- 21:50 production capacity can deliver doses
- 21:56 for countries that still don't have it and it can deliver boosters.
- 22:02 The problem is to prioritize delivery
- 22:07 for those who do not yet have access to vaccines
- 22:11 and for that purpose, what we are pressing for,
- 22:15 actually all four of us,
- 22:17 is disclosure of contracts,
- 22:21 transparency of who bought what, for what delivery date
- 22:27 and is this a good match of the objective we presented:
- 22:31 Vaccinate at least 40% of the world population
- 22:36 at the end of this year.
- 22:37 I can tell you that in our view,
- 22:40 transparency of contracts and delivery schedules
- 22:45 is going to go a long way to optimize the production capacity.
- 22:51 I want to make two more points
- 22:52 on the question of do we want to see more self-reliance?
- 23:00 The answer is yes.
- 23:02 We are very keen that this crisis turns into an opportunity
- 23:08 for Africa to be more self-reliant.
- 23:12 And in fact, I was very pleased
- 23:15 to learn from Senegal that are going to use
- 23:18 a portion of the special drawing rights
- 23:21 we have allocated to Senegal exactly for this purpose.
- 23:25 Our assessment is that if African countries
- 23:29 take 1 billion of the special drawing rights
- 23:33 to move it towards expanding production,
- 23:36 it can do a lot of good for the future.
- 23:39 My second point is to be clear that yes,
- 23:46 we do need more collaboration on all fronts.
- 23:51 Ngozi is the expert of the trade issue,
- 23:54 so I don't want to jump into her field,
- 23:58 but the simple final point I want to make here, Becky, is that
- 24:04 we are so much in this together, we can get out of it only together.
- 24:09 [BECKY ANDERSON] David, the world--
- 24:10 You make a very good point.
- 24:13 David, the World Bank has deployed over $157 billion dollars
- 24:18 to fight the impact of the pandemic.
- 24:21 This is, as I understand, the largest ever crisis response.
- 24:25 I just want our audience here
- 24:28 to get a sense of what financing instruments
- 24:31 you've used and what have been the results?
- 24:33 What's the learning here?
- 24:37 [DAVID MALPASS] This is a mix around the world
- 24:39 of loans and grants, and it goes to health,
- 24:42 it goes to education,
- 24:44 it goes to governments when they're making positive changes
- 24:48 in their laws that make them more attractive for business,
- 24:51 for setting up vaccine operations.
- 24:54 Part of that 157 billion is the supply of vaccines.
- 24:58 IFC, our private sector arm invests debt and equity
- 25:03 in vaccine manufacturing in Africa,
- 25:05 we're helping expand the Aspen Pharmaceutical in South Africa,
- 25:10 and we're helping research other sites
- 25:14 where vaccine manufacturing can occur.
- 25:16 So there's a range of investments made in development.
- 25:21 from that $157 billion dollars.
- 25:24 And remember, it's a leverage from donors.
- 25:28 Donors put money in and we borrow heavily against it
- 25:32 in capital markets.
- 25:33 It brings in people from around the world together
- 25:37 in sustainable development efforts.
- 25:39 Climate is a core one that's expanding rapidly as well.
- 25:43 [BECKY ANDERSON] Now, I understand that.
- 25:45 Ngozi, I just want to come to you at this point.
- 25:47 The WTO was created, of course, in 1995,
- 25:51 in part to address how trade could be used
- 25:54 to promote sustainable development.
- 25:57 I just wonder, this is a question that I've been asked myself
- 26:02 over the last 19 months,
- 26:04 whether the WTO has actually failed
- 26:08 low-income countries in this instance.
- 26:11 I just wonder what your response to that is.
- 26:14 [NGOZI OKONJO-IWEALA] I would say my response is no,
- 26:17 the WTO has not failed low-income countries in this instance,
- 26:21 this is actually an opportunity, a time
- 26:24 when the WTO and trade have responded very well.
- 26:29 People do not know it but last year,
- 26:33 as the value of trade fell by more than 7%,
- 26:38 the value of medical supplies and products
- 26:41 being treated rose by 16%.
- 26:44 and personal protective equipment by 50%.
- 26:47 What does this mean?
- 26:49 The trade backed by WTO's rules was actually moving goods around
- 26:56 to where they were needed.
- 26:57 Secondly, you mentioned the issue of the TRIPS earlier on.
- 27:02 You talked about the TRIPS waiver and the IP.
- 27:06 Of course, it's a WTO agreement.
- 27:09 More than 100 countries asked our members,
- 27:12 they are asking for a waiver of the intellectual properties rights
- 27:17 so they can have access to this to manufacture vaccines.
- 27:21 We have other members who think that if you do this,
- 27:26 it will get in the way of innovation.
- 27:29 So what are we trying to do?
- 27:31 Actually, there's an emerging consensus from our members now,
- 27:34 after a lot of debate and discussion,
- 27:37 that we need a solution to the IP problem.
- 27:40 People are dying and it's unconscionable.
- 27:43 We should not solve this.
- 27:45 As I said to you, there are discussions going on
- 27:49 for a pragmatic solution and I think we will get it, Becky.
- 27:52 This will allow developing countries
- 27:54 access to know-how technology transfer.
- 27:58 and then, at the same time, in a way that will show
- 28:02 those who have developed these vaccines that they will be protected.
- 28:06 We are not going to disincentivize research--
- 28:09 [BECKY ANDERSON] Ngozi, with respect,
- 28:11 there will be people who will be quite cynical
- 28:15 about what that solution might look like.
- 28:17 So can you just explain what you think it might look like?
- 28:21 [NGOZI OKONJO-IWEALA] This is something being discussed
- 28:25 at the moment by members,
- 28:27 so I cannot say what the ultimate solution will be.
- 28:32 I wanted to say that I'm pretty sure
- 28:34 it will allow better access than we have now,
- 28:37 from some provisions in our TRIPS Agreement
- 28:41 and make it easier for countries to get access.
- 28:44 We have to find the way of bridging this gap.
- 28:47 We all really agree it is not right that people should be dying.
- 28:51 We need to make sure that technology is transferred,
- 28:55 developing countries can manufacture.
- 28:57 I can't put on the table now because they're negotiating
- 29:01 it at this moment.
- 29:02 So I can't tell you the ultimate answer,
- 29:04 but I know it will come out to a pragmatic place.
- 29:08 [BECKY ANDERSON] Well, that's good to hear.
- 29:09 And I hope you will join us on.
- 29:16 Please go ahead.
- 29:18 [TEDROS ADHANOM GHEBREYESUS] Thank you.
- 29:19 So, on the IP,
- 29:23 I think the IP waiver would be very important.
- 29:27 And as global community, we should ask ourselves,
- 29:31 why do we have even the IP waiver as a legal instrument
- 29:35 if we're not going to use it in such unprecedented conditions?
- 29:39 Insufficient.
- 29:41 This pandemic happened more than 100 years after the 1918 flu.
- 29:48 The provision in the TRIPS Agreement was made in order to use it
- 29:55 in such situations, in emergencies.
- 29:58 So how can we say this should be an issue for debate?
- 30:06 When are we going to use the provision
- 30:10 if we cannot use it now?
- 30:13 My response is we should use the IP waiver now.
- 30:18 We should waive it because these are unprecedented times.
- 30:22 The other thing I would like to raise here is
- 30:25 we have spoken to some countries
- 30:28 who are not supporting the IP waiver
- 30:31 and spoken to manufacturers,
- 30:33 their responses is even if we waive the IP,
- 30:36 it will not be useful unless it's accompanied
- 30:39 by technology transfer.
- 30:41 Our response was,
- 30:43 “Okay, if what you're saying is the problem,
- 30:46 why don't you just waive and let's try if it works or not.”
- 30:52 Without trying you, you wouldn't know.
- 30:56 When you talk about technology transfer,
- 30:59 once you open or waive the IP, it can trigger technology transfer.
- 31:07 Those people who are working for those who control the IP will be free.
- 31:14 Since it will be legalized,
- 31:16 they will be free to migrate and help others,
- 31:19 or they can work part-time to transfer technology.
- 31:24 So it can happen if the IP is waived.
- 31:27 The other is, as Ngozi said, I fully agree,
- 31:32 we need incentives for the private sector.
- 31:35 We need to appreciate their role
- 31:37 because they have developed these vaccines in less than a year.
- 31:41 So in order not to affect the incentives for the long term,
- 31:47 the waiver could be for a very limited period of time.
- 31:50 It could be two years or three years
- 31:52 or until the end of the pandemic.
- 31:54 and it could focus on vaccines only.
- 31:57 But not waiving it now--
- 32:00 [BECKY ANDERSON] I understand.
- 32:01 [TEDROS ADHANOM GHEBREYESUS] when the situation is unprecedented,
- 32:03 the emergency is clear,
- 32:06 and the whole world is the hostage of this virus,
- 32:10 if we cannot waive it now then when.
- 32:12 To be honest, this is really something
- 32:16 where I can say humanity is failing miserably.
- 32:21 This is not acceptable.
- 32:23 It is in the interest of the manufacturers.
- 32:26 It's in the interest of each and every country
- 32:29 in the world to waive the IP,
- 32:31 do everything to increase production,
- 32:34 end this pandemic as soon as possible
- 32:36 and open up the world and release.
- 32:39 [BECKY ANDERSON] You heard that from the head of the WHO.
- 32:44 [NGOZI OKONJO-IWEALA] Can I just add to them just quickly.
- 32:48 We've been talking about waiving these IPs,
- 32:52 and I think that has brought people to the table.
- 32:55 I think let us see in a short while, hopefully maybe,
- 33:00 by our 12th Ministerial, which starts at the end of November,
- 33:05 both sides are talking to each other
- 33:07 and they should come up with a solution
- 33:09 that will give us light on this problem.
- 33:11 [BECKY ANDERSON] Let's hope that happens, Ngozi.
- 33:15 Go on Kristalina.
- 33:16 [KRISTALINA GEORGIEVA] If I may, just to say that
- 33:19 that touched on something very important.
- 33:21 It is the waiver, but then it is the technology ,
- 33:24 it is the skills and the capacity
- 33:26 to build that self-reliance,
- 33:29 and they have to all go hand in hand.
- 33:32 I'm actually encouraged to listen to some of the scientists
- 33:36 and some of the manufacturers that are recognizing
- 33:41 this is a terrible pandemic may not be the last one,
- 33:45 and if the world is to build strength, capacity
- 33:50 to face health risks in the future,
- 33:54 now is the time to approach this in a comprehensive manner.
- 33:59 We need resilience.
- 34:01 We need resilience for shocks to come.
- 34:03 [BECKY ANDERSON] I do want to talk about
- 34:05 that preparedness with all of you.
- 34:09 As we close out this extremely interesting session tonight,
- 34:15 before I do that,
- 34:17 it will come as no surprise to any of you
- 34:20 that we are not only dealing with the pandemic,
- 34:22 but also an infodemic
- 34:25 and a low level of trust in big societal institutions
- 34:29 such as the ones you are leading.
- 34:32 Kristalina, I'm going to start with you because just last night,
- 34:35 the IMF Board affirmed it's full confidence in your leadership,
- 34:39 after investigating your conduct while at the World Bank
- 34:43 related to data regarding China's economic performance.
- 34:47 I want to give you an opportunity
- 34:49 to respond to that decision
- 34:52 and ask you whether you think this episode
- 34:55 has further eroded trust in institutions such as the IMF
- 34:59 and entangled you personally
- 35:02 in the wider geopolitical rivalry between the US and China.
- 35:07 [KRISTALINA GEORGIEVA] Becky, I'm so glad you asked.
- 35:12 The Board of the IMF
- 35:16 in a comprehensive and impartial process,
- 35:21 reviewed the evidence,
- 35:22 and it concluded that it has full confidence
- 35:26 in my leadership at the IMF.
- 35:28 So I can rally the fabulous [inaudible] staff of the IMF
- 35:35 work with our partners, those who are on this panel
- 35:38 to address the tough challenges we face.
- 35:42 We talk about the pandemic, we have climate,
- 35:44 we have the issue of inequality, and of course,
- 35:47 I take it to heart that we have to strive always
- 35:52 to demonstrate that what we do
- 35:55 touches positively the lives of people.
- 35:59 And I take pride of what we have done.
- 36:02 The IMF in these two years
- 36:05 to mobilize incredibly strongly to help our members
- 36:07 incredibly strongly to help our members.
- 36:11 And I am confident that you would see the IMF to be
- 36:17 that beacon of integrity of our data and research
- 36:21 as we have always been.
- 36:23 You are right.
- 36:25 We have to always work for the public trust.
- 36:28 That is what they have been doing for 40 years.
- 36:30 [BECKY ANDERSON] And you've been asking for accountability
- 36:33 and transparency tonight on this very panel.
- 36:36 David, I have to come to you.
- 36:37 The credibility of international organizations has been eroded
- 36:41 due to various controversies, not least that of the IMF firm
- 36:46 or the World Bank and the issue that we've just been discussing
- 36:50 with Kristalina.
- 36:51 Does this trust need to be rebuilt, sir?
- 36:54 [DAVID MALPASS] I'm looking forward
- 36:56 to strong collaboration continued with IMF,
- 36:59 with Kristalina, with Ngozi and Tedros.
- 37:03 And one thing I would say
- 37:04 is you have with you today
- 37:07 four really hard working public officials
- 37:12 that are watched every hour every day, every week.
- 37:17 And so we're working hard in order to get the job done.
- 37:23 I know my day is full of chances to try to make a difference
- 37:28 and to help people.
- 37:29 And I look forward to having as much integrity,
- 37:33 accountability in all of those affairs
- 37:35 as we can, World Bank's doing quality research into the future.
- 37:40 And it's vital as part of the development effort.
- 37:43 [BECKY ANDERSON] What are the learnings out of this episode, David?
- 37:48 [DAVID MALPASS] Learning is constantly review
- 37:52 the quality of your products, make them better, build them hard,
- 37:56 and keep focused on getting good development outcomes for countries.
- 38:00 [BECKY ANDERSON] How do we prepare
- 38:02 for future potential crises, Ngozi?
- 38:06 [DAVID MALPASS] And I was going to say
- 38:09 preparedness is a core part of World Bank and of IDA.
- 38:12 We fast-tracked our front, loaded our IDA into the crisis,
- 38:18 and that's been vital
- 38:19 in delivering as many programs as we have.
- 38:22 [BECKY ANDERSON] Ngozi.
- 38:24 [NGOZI OKONJO-IWEALA] Yeah.
- 38:25 Becky, thank you.
- 38:26 Actually, to prepare for the next crises,
- 38:29 I have to tell you, the G20 Finance Ministers
- 38:32 set up a task force to look into this.
- 38:35 And this was coached by myself, by Larry Summers,
- 38:38 and Tharman Shanmugaratnam, the Senior Minister of Singapore.
- 38:44 And we found four major gaps in pandemic preparedness.
- 38:48 We found that there is a gap
- 38:50 in globally networked surveillance and research
- 38:54 to prevent and detect emerging infectious diseases.
- 38:58 We found a second gap in resilient national systems.
- 39:01 That means that our health systems when this happened
- 39:05 were just not prepared both in rich and poor countries.
- 39:08 We found that there was not an adequate supply
- 39:11 of medical tools and counter measures
- 39:14 to deal with this pandemic.
- 39:16 And as we've just been talking
- 39:18 also inequity of access, the world was not prepared
- 39:22 for access to this.
- 39:23 And the last gap was in global governance.
- 39:25 There just wasn't a mechanism to coordinate
- 39:28 all the different organizations, to make sure that funding
- 39:32 came on time,
- 39:33 and that the international financial architecture worked
- 39:36 and there was no organization to really be accountable
- 39:40 for all the outcomes.
- 39:41 We made three recommendations to be prepared,
- 39:44 and I'll be very fast.
- 39:46 One is that increased--
- 39:47 We all have to increase spending domestically to strengthen
- 39:51 our health systems
- 39:52 in low-income countries and middle-income countries,
- 39:55 we've actually suggested one percentage point of GDP extra
- 39:59 in spending over the next five years in order to be prepared.
- 40:04 In addition to this,
- 40:05 we're also saying we need increased international spending
- 40:09 because there's a public good aspect
- 40:11 for managing the pandemic.
- 40:13 We recommend that $75 billion over the next five years,
- 40:17 15 billion a year of which 10 billion
- 40:20 should go into a global health threat fund.
- 40:23 And finally, we've recommended improved global governance,
- 40:27 a global health threat fund,
- 40:30 a global health threat board
- 40:33 that would oversee and coordinate a preparedness
- 40:37 for the next pandemic, and the spending.
- 40:39 [BECKY ANDERSON] Tedros, I do want
- 40:41 to get your perspective.
- 40:42 I've also got a question from an interested audience member
- 40:47 watching this discussion who says
- 40:50 the WHO is at the forefront of global health.
- 40:53 And Renee asks: Will COVID lead to the reform
- 40:57 of management and investment in medical and health research?
- 41:02 [ENDING THE PANDEMIC: THE ROAD TO AN INCLUSIVE RECOVERY]
- 41:05 [TEDROS ADHANOM GHEBREYESUS] The answer is yes, it will.
- 41:08 As I said earlier, this pandemic is unprecedented
- 41:12 and we're documenting all lessons that we need to learn.
- 41:16 Part of it, which Ngozi said
- 41:18 and all these recommendations should be implemented.
- 41:21 I think this will help us if we can learn
- 41:26 from this pandemic properly
- 41:28 and implement the recommendations,
- 41:30 that we'd be different and we can be better prepared.
- 41:34 One thing I would like to add to this is
- 41:36 the Pandemic Treaty will be very important or Pandemic Agreement.
- 41:41 We have seen many challenges
- 41:44 that could have been addressed if we had a framework
- 41:48 or a legal instrument that could guide us.
- 41:51 So that would be very key
- 41:54 by the way, in the change
- 41:56 we will have to prepare the world in a better way.
- 41:58 The Pandemic Treaty or Pandemic Agreement.
- 42:03 [BECKY ANDERSON] Kristalina, finally,
- 42:04 I just wanted to come to you.
- 42:06 You came to the IMF wanting to talk about gender pay parity,
- 42:10 doing more to tackle the climate crisis,
- 42:13 talking more about income equality.
- 42:17 You couldn't have known quite what was coming down the pipe
- 42:22 with regard the COVID pandemic.
- 42:24 You've gone beyond this narrow focus
- 42:28 and adopted a much more,
- 42:29 as some would describe it, holistic approach,
- 42:34 which is exactly what many of us have said that we needed.
- 42:37 I wonder whether, to a certain extent, you feel
- 42:40 as if that, maybe, what got you into hot water recently,
- 42:44 but also just get your perspective on ultimately,
- 42:47 what the learnings are here
- 42:49 to ensure that we are more prepared
- 42:51 for any eventualities going forward.
- 42:54 [KRISTALINA GEORGIEVA] We are living
- 42:56 in a fast changing world, Becky,
- 43:00 and we have to anticipate
- 43:04 what's next.
- 43:05 And then, have the agility
- 43:08 to prevent crises,
- 43:12 to respond quickly,
- 43:14 to target the most vulnerable,
- 43:17 and to do so,
- 43:20 as Ngozi was saying, across the board.
- 43:23 We need to scan the horizon better.
- 43:26 We have to have better monitoring of these risks
- 43:29 and then, the extra capacity is necessary to step up.
- 43:35 But above all, we need to work on countries to have
- 43:40 strong institutions, educated people that are healthy,
- 43:46 capable to adjust to these shocks,
- 43:50 to hear about the agility and capacity
- 43:55 of our planet to absorb these shocks
- 43:59 and to be with institutions everywhere that have the skills
- 44:05 to lead towards
- 44:08 a more sustainable, more equitable future.
- 44:12 What does it mean if you compare with the pandemic?
- 44:15 Who did the pandemic hit the hardest?
- 44:19 People with weak immune systems, the same way countries
- 44:24 with weak institutions, with weak immune systems
- 44:28 get hit hardest.
- 44:30 So working relentlessly to build
- 44:32 that institutional capacity
- 44:35 to have development that gives jobs to people,
- 44:39 makes them able to have good business opportunities.
- 44:44 This is what matters.
- 44:47 To turn it into the language of our conversation today.
- 44:52 Building resilience is about...
- 44:55 People, institutions and our planet.
- 45:00 [BECKY ANDERSON] Having you all with us today
- 45:04 has been extremely important.
- 45:06 I know that the audience listening to this
- 45:09 will have found this incredibly valuable.
- 45:12 And, David, you're right.
- 45:13 All of you are extremely hard workers.
- 45:16 It is so important that the conversation
- 45:21 is out there, that the challenges that you face are clear
- 45:25 and that the goals that you have set yourself
- 45:27 with this multi-leader task force are clear.
- 45:33 And we hope, achievable,
- 45:34 we thank you very much indeed, all of you for joining us today.
- 45:38 It's been fascinating.
- 45:41 And let's hope that we are not talking in 19 months' time
- 45:47 about the very same issue of vaccine inequality
- 45:50 because that would be terrible.
- 45:53 Thank you very much indeed, for joining us today.
- 45:55 All of you. I'm Becky Anderson.
- 45:57 Good night.
- 46:02 [Upbeat Music]
- 46:13 [ANNUAL MEETINGS 2021]
- 46:14 [WORLD BANK GROUP INTERNATIONAL MONETARY FUND]
- 46:16 [ENDING THE PANDEMIC: THE ROAD TO AN INCLUSIVE RECOVERY]
- 46:24 [JULIETTE POWELL, AUTHOR AND BUSINESS COMMENTATOR] And welcome.
- 46:26 We are live from World Bank Group headquarters in Washington, DC.
- 46:31 I'm Juliette Powell and I'll be your host today
- 46:34 as we continue our discussion on how to end
- 46:37 this pandemic of a truly inclusive recovery.
- 46:41 We've just heard from the leaders of the task force.
- 46:43 And over the next half hour,
- 46:45 we'll be digging deeper into some of the issues and asking
- 46:49 what can be done to accelerate access to vaccines
- 46:52 for developing countries,
- 46:53 And how are the private sector and civil society
- 46:57 helping to address this challenge?
- 46:58 We'll be joined by leaders and experts from across the globe.
- 47:02 Here's a quick look ahead.
- 47:05 [Upbeat Music]
- 47:16 [ANNUAL MEETINGS 2021]
- 47:17 [WORLD BANK GROUP INTERNATIONAL MONETARY FUND]
- 47:20 [COMING UP] [ENDING THE PANDEMIC: THE ROAD TO AN INCLUSIVE RECOVERY]
- 47:24 [MAKHTAR DIOP, MANAGING DIRECTOR, IFC]
- 47:26 [NARENDER MANTENA, HEAD OF GLOBAL STRATEGY, BIOLOGICAL E. LIMITED]
- 47:29 [STRIVE MASIYIWA, CHAIRMAN, ECONET & AFRICAN UNION SPECIAL ENVOY]
- 47:33 [DR. AHMED OGWELL OUMA DEPUTY DIRECTOR, AFRICA CDC]
- 47:40 [NADIA DAAR, OXFAM, WASHINGTON DC]
- 47:42 [PRISCILLA NYAABA, YOUTH HARVEST FOUNDATION, GHANA]
- 47:47 [MAMTA MURTHI, VICE PRESIDENT HUMAN DEVELOPMENT, WORLD BANK]
- 47:50 [STEPHANIE VON FRIEDEBURG, SENIOR VICE PRESIDENT OPERATIONS, IFC]
- 47:56 [JULIETTE POWELL] Every single one of us
- 47:58 has been affected by this pandemic and getting through it is
- 48:01 a shared global priority and our responsibility.
- 48:04 We're hearing from people affected in different ways
- 48:07 from youth, civil society organizations
- 48:10 as well as global leaders.
- 48:12 So let's start in the Philippines.
- 48:13 Like in most places, the pandemic shut down schools, markets,
- 48:18 transportation, leaving people desperate
- 48:20 for an end to the threat of COVID-19.
- 48:23 We asked one mother and daughter to share their experiences
- 48:26 and their hopes,
- 48:28 now that vaccines have begun to reach those most in need.
- 48:33 [ANNUAL MEETINGS 2021 WASHINGTON DC]
- 48:36 [Upbeat Music]
- 48:42 The World Bank Group is funding 13 million doses
- 48:44 of COVID-19 vaccine for the Philippines
- 48:47 The first batch arrived in June 2021
- 48:48 with the rest expected by the end of the year.
- 48:51 [DAUGHTER] On TV, in the news, on the internet, they said ta lot of people were dying because of this sickness
- 48:59 And that's what scared us.
- 49:01 [MOTHER] Of course, I was scared - that my kids would get it, my grandchildren would get it, especially us, we're older
- 49:08 [DAUGHTER] Our school announced enrolment would be online instead.
- 49:12 Our internet connection wasn't that strong and their website
- 49:17 kept crashing so I couldn't enrol properly.
- 49:20 There have been so many challenges.
- 49:21 I also couldn't work because there were no rides, I couldn't commute, there was no transportation.
- 49:31 Mom and dad also stopped working then,
- 49:35 [MOTHER] My job was to take care of kids, before when there was no pandemic.
- 49:41 But now, not anymore, because their parents weren't going to work.
- 49:46 -It was hard to know how we'd feed ourselves.
- 49:51 [Upbeat Music]
- 49:57 The World Bank Group is funding 13 million doses
- 49:59 of COVID-19 vaccine for the Philippines
- 50:01 The first batch arrived in June 2021
- 50:03 with the rest expected by the end of the year.
- 50:06 [DAUGHTER] I'm happy mom is vaccinated now. It's her first dose.
- 50:09 She had doubts at first but my sister and I told her that side effects are normal.
- 50:16 [MOTHER] I'm OK now. I'm happy because my children have work and I've also been vaccinated.
- 50:21 My husband has work too.
- 50:23 Things are not as hard for us anymore.
- 50:25 [DAUGHTER] My dream is to finish studying, to keep going without having to stop.
- 50:32 And then to become an HR manager. That's what I really want.
- 50:37 The World Bank Group is boosting private sector vaccine manufacturing capacity globally.
- 50:40 [DAUGHTER] I'm happy that (vaccines) have arrived in the Philippines.
- 50:43 Some people have already been vaccinated and it keeps going
- 50:46 What I want to say is that I hope we can speed up vaccination efforts
- 50:52 so we can end this difficult pandemic
- 50:56 and we can continue
- 51:00 chasing our dreams.
- 51:04 #vaccines4all
- 51:11 [ANNUAL MEETINGS 2021 WASHINGTON DC]
- 51:13 [WOMAN] Salam. I'm [inaudible] from Almaty, and you are watching
- 51:18 the World Bank Group-IMF Annual Meeting.
- 51:24 [JULIETTE POWELL] What an incredible story of survival and hope.
- 51:27 We're streaming this event
- 51:29 in English, French, Spanish and Arabic on World Bank Live
- 51:33 and on our social media channels and to tell us
- 51:36 how you can finally get involved,
- 51:38 I'm joined now by Sri Sridhar. Welcome, Sri.
- 51:41 [SRI SRIDHAR] Thanks, Juliette.
- 51:42 [JULIETTE POWELL] So we had a chance to listen
- 51:44 to the task force leaders talking about all of those challenges.
- 51:47 How about getting the people that are watching involved as well?
- 51:50 [SRI SRIDHAR] Absolutely.
- 51:51 So similar to yesterday, you can follow us
- 51:53 on our social media channels.
- 51:54 We're on Facebook, Twitter, and Instagram.
- 51:57 You can also share comments at any time
- 51:59 using the hashtag for today's event, which is #vaccinesforall.
- 52:02 And you can also post your questions and comments
- 52:04 at any time on live.worldbank.org.
- 52:07 So really a lot of ways for everyone
- 52:09 to kind of get involved and join the conversation.
- 52:11 Now, you did mention that the event is being streamed
- 52:13 in English, Spanish, French and Arabic.
- 52:15 And the good news is we've got
- 52:17 experts standing by in all four languages,
- 52:19 and they're working hard to answer as many questions as possible.
- 52:22 We can see some of them right here.
- 52:24 And I know that some of the most popular questions
- 52:27 I think are gonna be put to a couple of the senior experts
- 52:29 later today.
- 52:30 [JULIETTE POWELL] Yeah, we're very, very lucky.
- 52:31 We're gonna be joined a little bit later on by Mamta Murthi
- 52:35 He's the Bank's Vice President of Human Development.
- 52:38 We've also got Stephanie von Friedeburg.
- 52:40 She-- You might even know her.
- 52:42 She's a Senior Vice President of Operations for IFC,
- 52:45 and we've got our viewers.
- 52:47 Now, how do we get them involved in the poll?
- 52:49 [SRI SRIDHAR] Yeah. So the poll for today asks:
- 52:52 What is most important to ensure equitable
- 52:55 and successful COVID-19 vaccine deployment?
- 52:58 And there are four options.
- 53:00 The first, is it by having an adequate stock of vaccines?
- 53:03 A sufficiently funded, resilient and inclusive health system.
- 53:07 Enough equipment and trained public health personnel? Or is it
- 53:10 by having engagement of local community leaders and organizations?
- 53:15 So once again, the poll for today asks:
- 53:17 What is most important to ensure equitable
- 53:19 and successful COVID-19 vaccine deployment.
- 53:22 And the choices are by having an adequate stock of vaccines.
- 53:26 A sufficiently funded, resilient and inclusive health system.
- 53:30 Enough equipment and trained public health personnel, or
- 53:33 is it engagement of local community leaders and organizations?
- 53:36 So for those of you folks who are tuning in head on over
- 53:39 to live.worldbank.org and cast your vote before the poll closes.
- 53:43 [JULIETTE POWELL] Thanks so much Sri.
- 53:44 I really look forward to hearing what the results are going to be.
- 53:47 We're gonna find out by the end of the show today.
- 53:50 -Thanks. -Thanks, Juliette.
- 53:54 [JULIETTE POWELL] Now the private sector is playing a very
- 53:57 important role in pandemic response,
- 53:59 vaccine production and distribution.
- 54:01 To learn more about what the private sector
- 54:04 can and is doing to meet vaccine needs,
- 54:07 and the challenges faced
- 54:08 IFC Manager Director, Makthar Diop, is joined
- 54:11 in discussion by two leaders in the health field.
- 54:14 [MAKTHAR DIOP] I'm joined by two great leaders
- 54:17 who are in the area, each making a huge difference.
- 54:21 Strive Masiyiwa is a founder of Econet
- 54:25 a leader company in the mobile-- digital sector in Africa
- 54:30 but also he's-- he has been working
- 54:32 a lot on vaccine, and he's a Special Envoy
- 54:34 from the African Union to help really bring
- 54:37 the private sector in producing more vaccine in Africa.
- 54:40 Narender is a CEO of [inaudible].
- 54:43 Well, as you know, a lot of the production
- 54:45 of vaccine has been coming from India and the research
- 54:48 also in this area has been going on.
- 54:50 We have today's situation
- 54:53 where only 4% of the population in Africa is vaccinated.
- 54:56 We have a lot of vaccine inequity
- 54:59 that has been discussed and talked about.
- 55:01 And today we would like to discuss
- 55:03 what we can do to solve that issue.
- 55:05 And these two leaders,
- 55:06 will give us the insight and the idea
- 55:09 about how we can go about it.
- 55:11 Let me start first with Strive.
- 55:14 So have you been involved very much in making
- 55:18 sure that we increase the supply of vaccine in Africa.
- 55:22 So what needs to be done
- 55:24 to increase the supply of vaccine in Africa?
- 55:27 [STRIVE MASIYIWA] Thank you very much, Makhtar.
- 55:29 It's good to see you, my dear brother.
- 55:31 My job as the African Union Special Envoy
- 55:36 is to coordinate the acquisition of vaccines.
- 55:40 My primary-- I
- 55:43 I coordinate the task force made up of ministers
- 55:47 and health specialists,
- 55:50 including the Africa Center for Disease Control,
- 55:54 to purchase vaccines.
- 55:57 We have created a special purpose vehicle called
- 56:01 the Africa Vaccine Acquisition Trust,
- 56:05 which we funded
- 56:08 with a 2 billion dollar facility.
- 56:13 We also have secured, as you know,
- 56:17 over 4 billion dollars of support from the World Bank
- 56:21 for the member states to buy vaccines.
- 56:23 This is the first time anything of this scale
- 56:27 has ever been done where Africa is buying together
- 56:31 vaccines on a major scale.
- 56:34 So I've gotta-- Although I don't come from the sector,
- 56:38 I've picked up some idea what the challenges are,
- 56:41 and I hope we'll be able to discuss them as we proceed
- 56:47 But really, that is my job.
- 56:51 And it's been-- The challenge for us
- 56:55 has been to secure supply
- 56:58 because Africa made the mistake
- 57:02 of seeding manufacturing of vaccines
- 57:06 to other regions of the world.
- 57:08 And this is the thing that we have to fix,
- 57:11 that vaccines must be manufactured on the African soil.
- 57:16 [MAKHTAR DIOP] Thank you very much, Strive.
- 57:18 I come back to you and ask you, what are the conditions
- 57:21 for it to happen?
- 57:22 And with your huge experience in the private sector
- 57:27 in Africa, what needs to be done to attract private sector in vaccine?
- 57:31 I'll come back to you to that after I ask Narender
- 57:34 who is from India, where had they been able to do that?
- 57:37 So how have we been able to do that in India?
- 57:41 And what are the three lessons
- 57:43 that you can draw from your experience
- 57:46 such-- can be useful
- 57:47 for the part of the world who wants to do the same thing.
- 57:49 [NARENDER MANTENA] And India is a different story.
- 57:53 I think it's a long story. And quickly...
- 57:56 The Indian private sector manufacturing started in the 60s
- 58:00 with the Serum Institute in our company in a small way.
- 58:03 But the real [inaudible] for the Indian vaccine manufacturing
- 58:06 didn't happen until Gavi was formed
- 58:09 in the late 90s and 2000s,
- 58:12 there were incentives created by the Gates Foundation in WHO
- 58:17 to prequalify companies out of India,
- 58:20 and they started supplying the global market
- 58:22 that included Africa and other nations.
- 58:25 I think that gave the [inaudible]
- 58:28 of large capacities in India
- 58:30 that we're able to utilize now.
- 58:34 On top of that, India also had large biologics,
- 58:38 and biosimilar market, and these facilities have been repurposed.
- 58:43 So I think it's not one simple story.
- 58:46 It is a combination of an evolution of a domestic market
- 58:51 incentivized by global markets in UNICEF and Gavi,
- 58:55 and complemented with the pharmaceutical markets
- 58:58 that allowed India to be able to respond to the pandemic
- 59:01 in its own way.
- 59:02 In terms of lessons, I think that this lesson is
- 59:06 probably not the right way to go
- 59:08 because it takes a long time to get there,
- 59:10 and I'm sure Strive will talk about it.
- 59:12 But-- continents like Africa
- 59:16 do have the ability to create a market of its own
- 59:20 and by centralized procurement
- 59:23 to incentivize manufacturers to come into Africa.
- 59:26 I think the challenge of the pandemic is
- 59:28 slightly different, because if you look at how the pandemic
- 59:32 has been addressed, not only in India but in US and Europe,
- 59:37 they had to leverage pharmaceutical facilities
- 59:39 to be able to scale up.
- 59:41 So...
- 59:42 creating a pandemic-ready infrastructure
- 59:45 will be a different challenge that we have to figure out
- 59:48 how to address.
- 59:50 So I think the three lessons would be domestic market
- 59:54 for Africa, for African manufacturers
- 59:58 incentivizing either with a push and pull funding
- 01:00:02 to make the prices affordable and to create
- 01:00:06 pandemic manufacturing infrastructure
- 01:00:09 and funding it on a regular basis.
- 01:00:11 Not knowing when the next pandemic will hit
- 01:00:14 would be the lessons, they're not directly from India.
- 01:00:17 But India was able to do it organically.
- 01:00:20 But that's what I believe needs to be done in other areas.
- 01:00:24 [MAKHTAR DIOP] Thank you very much.
- 01:00:25 Let me turn to my friend Strive.
- 01:00:27 So having been one as a precursor in an area
- 01:00:30 where this was quite complicated at the beginning, digital.
- 01:00:33 Not a lot of people wanted to put their money in Africa
- 01:00:36 take that risk and be able to price the risk,
- 01:00:39 understanding and to be able to address the challenges
- 01:00:42 that people-- investors were facing at that time.
- 01:00:46 Build on your experience in the digital, what you think,
- 01:00:51 from what you heard from Narender, from your own experience
- 01:00:55 will be the condition to attract more private investment
- 01:00:58 in vaccine, in Africa.
- 01:01:01 [STRIVE MASIYIWA] Well, you know, I think
- 01:01:04 it's very important what my colleague just said,
- 01:01:09 it's very profound
- 01:01:12 because I came to the same conclusion.
- 01:01:16 But it was institutions like Gavi
- 01:01:20 that are responsible for the crisis in Africa
- 01:01:26 because what they did was to create
- 01:01:28 a public market in the purchase of vaccines
- 01:01:33 and then to strategically shift it to India.
- 01:01:36 So there is no way that African industrialists
- 01:01:40 could respond because the buyer--
- 01:01:44 decided that Africa's vaccines would come from India.
- 01:01:49 This was a strategic decision
- 01:01:53 in which Africans had no say.
- 01:01:57 And so we find ourselves in this situation
- 01:02:00 whereby when we found-- when we got into a crisis
- 01:02:04 and India was in the same crisis,
- 01:02:07 India said it would take care of its own people
- 01:02:12 and we went to the back of the queue.
- 01:02:15 Africans are really mad about this.
- 01:02:18 Okay?
- 01:02:19 And I have told Gavi and UNICEF and even Gates
- 01:02:24 that this was wrong.
- 01:02:25 We need to correct this.
- 01:02:28 I'm sorry, but we got a big blunt about it.
- 01:02:31 African industrialists can do exactly what Indian industrialists can do.
- 01:02:35 Okay?
- 01:02:37 We have companies in Africa who were denied
- 01:02:40 the opportunities that were extended
- 01:02:43 to Indian manufacturers,
- 01:02:44 and that's why we're in this mess.
- 01:02:47 And we have to correct it.
- 01:02:50 We admire what has happened in India,
- 01:02:52 but we have to do the same
- 01:02:54 because we exported to India millions of jobs
- 01:02:59 in the production of vaccines.
- 01:03:01 Okay?
- 01:03:02 And I have said this and I will say it again.
- 01:03:05 We have to fix it.
- 01:03:08 How industrialists are capable of producing vaccines.
- 01:03:14 This is not a complicated thing.
- 01:03:16 It's the same technology that they have access to.
- 01:03:20 We know from Aspen
- 01:03:23 and Biovac and Dakar Institute
- 01:03:27 that had the same support
- 01:03:30 being given to them by the likes of Gavi and UNICEF,
- 01:03:35 we would not be in this mess.
- 01:03:38 So I will say it and say it again.
- 01:03:42 [MAKHTAR DIOP] So, I thank you very much.
- 01:03:43 But I think that there is an opportunity for convergence here.
- 01:03:47 And Narender, I know that you are looking also
- 01:03:50 at working in other places outside from India.
- 01:03:55 And I think, maybe, this is an opportunity
- 01:03:58 to invest in Africa because there is need,
- 01:04:02 there is a market, as you said, and there is a willingness
- 01:04:05 to build that ecosystem in some of the countries.
- 01:04:08 Would you be interested
- 01:04:09 if industrialists from Africa, as I've said, were approaching you
- 01:04:15 and said, let's do a joint venture, and invest on the continent?
- 01:04:19 [NARENDER MANTENA] Absolutely.
- 01:04:21 I think for us.
- 01:04:22 And as I said, I think that I completely agree with Strive
- 01:04:28 on the outcome of what Gavi did with respect to the pandemic.
- 01:04:32 Now, whether Gavi could have foresaw it
- 01:04:34 this kind of a pandemic. I mean, that's debatable.
- 01:04:38 I think we have never--
- 01:04:39 the world has never seen a pandemic like this.
- 01:04:41 Where essentially everybody had to get vaccinated.
- 01:04:45 So having said that to answer your question,
- 01:04:48 I think we definitely look at Africa.
- 01:04:50 I think for us, you know...
- 01:04:53 It is a market of importance we have been servicing through Gavi
- 01:04:57 but if it necessitates-- not necessitates-- It is.
- 01:05:02 The pandemic has taught us that,
- 01:05:05 you know, while we appreciate India looking out for India,
- 01:05:09 as a private company,
- 01:05:11 we don't feel good when people that have supported us globally,
- 01:05:16 that is [inaudible], Africa.
- 01:05:17 We're not able to service.
- 01:05:19 So it's not a good feeling
- 01:05:21 when you are not able to give back to countries
- 01:05:24 that have supported us for a long time.
- 01:05:26 But unfortunately, it's not in our hands
- 01:05:29 but to answer your question, yes, I think that we would be very open
- 01:05:31 as a company to do it ourselves.
- 01:05:34 Our preference is to find partners that we can do it with,
- 01:05:37 and then we'd be very open, and we're in fact, actually,
- 01:05:39 where we are slowly initiating discussions around it.
- 01:05:43 [MAKHTAR DIOP] I think that this conversation
- 01:05:46 was aiming at creating this link.
- 01:05:49 And I think that we are building it together, the three of us.
- 01:05:52 So, Strive to you, please.
- 01:05:53 [STRIVE MASIYIWA] Well, when I met with you, recall,
- 01:05:57 I said the future for you
- 01:06:00 is to manufacture from Africa.
- 01:06:03 You can own a hundred percent.
- 01:06:06 I will personally buy, you name the African country.
- 01:06:10 I'll buy the land and give it to you for free
- 01:06:12 myself with my own money.
- 01:06:14 Okay?
- 01:06:15 As a gift, you must manufacture from Africa.
- 01:06:19 And the future.
- 01:06:21 Is that's what's going to happen
- 01:06:23 When Sinophone came to me, I said you manufacture from Africa.
- 01:06:28 Otherwise, you don't get orders.
- 01:06:29 They are now manufacturing in Africa.
- 01:06:32 I'll give them an order.
- 01:06:33 If you want orders from us as AVAT,
- 01:06:36 you come and manufacture from Africa,
- 01:06:38 you choose your country, you do what you want.
- 01:06:41 You can have it a hundred percent whatever you want.
- 01:06:45 But you do it from Africa.
- 01:06:46 And we are going to start putting a lot of pressure on Gavi.
- 01:06:51 Every single contract that Gabi now signs.
- 01:06:55 If it is to supply Africa,
- 01:06:57 they must justify
- 01:07:00 where that-- why that production did not come from Africa.
- 01:07:04 Okay. It's-- It's going--
- 01:07:06 This is the result
- 01:07:08 of the decision that was taken in India to just cut us off.
- 01:07:13 You cut us off in March.
- 01:07:14 Politically, they said no more vaccines.
- 01:07:17 We'll deliver to you when we have delivered to our own people,
- 01:07:21 which is what Europe did to us.
- 01:07:24 Okay, so we've-- I've said it to the Indian manufacturers.
- 01:07:28 You are welcome.
- 01:07:30 You, Serum Institute, buyer.
- 01:07:32 Come, come.
- 01:07:34 But you make from Africa, so we can also have jobs.
- 01:07:38 And next time, no one can cut us off politically.
- 01:07:42 [MAKHTAR DIOP] Thank you so very much, my friend.
- 01:07:44 This is a wonderful conversation.
- 01:07:46 But unfortunately, as I say,
- 01:07:48 in my country every good-- all good things have an end.
- 01:07:51 and we have, too.
- 01:07:52 But I think that we made a lot of progress, Strive and Narender,
- 01:07:55 thank you very much.
- 01:07:57 Often we say, as these discussions, meetings leading to something.
- 01:08:01 Today, I have the feeling
- 01:08:02 that it leads to something very concrete and precise.
- 01:08:04 Strive you made a call for investment,
- 01:08:07 investing in Africa.
- 01:08:09 Narender says yes. "I'm looking at it."
- 01:08:11 "I'm interested in doing that."
- 01:08:13 So I think that IFC would be working with both of you
- 01:08:17 we'd be very happy to be your partner in doing
- 01:08:20 that together and creating those opportunities.
- 01:08:24 So this is for us, a great outcome of the conversation.
- 01:08:28 And we continue and let me say a last word.
- 01:08:31 This is just the beginning for us
- 01:08:34 of investing in the highest sector in Africa.
- 01:08:37 We have a lot of other health challenges to deal with.
- 01:08:40 Diabetes is becoming an increasing problem in Africa.
- 01:08:44 I brought pressure.
- 01:08:45 All these drugs, which are so necessary to improve
- 01:08:48 the half of African population,
- 01:08:50 need to be built cheaply,
- 01:08:52 make it accessible to people of Africa.
- 01:08:55 But I think that this conversation that we started,
- 01:08:57 for me, is the beginning of a bright future.
- 01:09:01 And I would like to thank you for joining me.
- 01:09:04 -Yes, please, Strive. -[STRIVE MASIYIWA] Let me just say one quick thing.
- 01:09:07 I'm not in the vaccine industry.
- 01:09:09 I'm a tech guy.
- 01:09:11 Okay?
- 01:09:12 I will help you find partners if you want.
- 01:09:15 You can be a hundred percent.
- 01:09:17 You are welcome.
- 01:09:18 Come and produce in Africa.
- 01:09:21 [MAKHTAR DIOP] Beautiful word to conclude, Strive.
- 01:09:23 Thank you so much, all of you.
- 01:09:25 And be safe.
- 01:09:27 Thank you so much.
- 01:09:30 [MAN] Hi, I'm [inaudible] from Dhaka.
- 01:09:32 And you're watching the World Bank Group-IMF Annual Meetings
- 01:09:37 [JULIETTE POWELL] If you're just joining us, I'm Juliette Powell.
- 01:09:41 And you're watching
- 01:09:42 Ending the Pandemic: The Road to an Inclusive Recovery.
- 01:09:45 It's been incredible.
- 01:09:47 Listening to Makhtar and his guests discuss
- 01:09:49 the vaccine challenge in Africa.
- 01:09:51 Now, we all know that the situation varies across the continent,
- 01:09:54 but on average,
- 01:09:56 less than five percent of the African population
- 01:09:59 is vaccinated, and that's why the World Bank
- 01:10:01 has intensified its technical and financial support in the region.
- 01:10:05 So let's take a look at how that's actually making a difference
- 01:10:08 to the health systems
- 01:10:10 and particularly, for the people in Cote d'Ivoire.
- 01:10:14 [ANNUAL MEETINGS 2021 WASHINGTON DC]
- 01:10:17 When COVID-19 hit Africa, healthcare systems struggled to cope
- 01:10:25 [WOMAN] At the beginning of the pandemic,
- 01:10:27 it was very difficult for ourselves, as health care personnel
- 01:10:32 in our relationships with our relatives, friends, clients, and staff,
- 01:10:39 given the fact that the disease, it's very contagious
- 01:10:43 In Cote d'Ivoire the World Bank Group supported a program that is:
- 01:10:47 Operating mobile clinics, deploying vaccines in 113 health districts
- 01:10:50 diversifying vaccine supply sources, raising awareness.
- 01:10:53 [MAN] Like most people,
- 01:10:54 I sensed that there was a slowdown across the board in 2020.
- 01:11:02 I even had to stay with my children for some time to teach them at home
- 01:11:07 Then, on top of that, there are all these stories that you hear from other people, and reports from various sources
- 01:11:14 and from the media.
- 01:11:16 So, once I realized the gravity of the situation I decided to go and get the vaccine
- 01:11:23 Within 4 weeks, the number of people vaccinated increased ten-fold
- 01:11:29 Giving people hope for the future
- 01:11:33 [WOMAN] The more people are vaccinated, the faster we will stop the virus from circulating.
- 01:11:40 And then people will start to resume their regular activities,
- 01:11:44 because I'm sure you will agree with me that since the outbreak of the disease there have been so many things that we can no longer do.
- 01:11:50 We need to get back to a normal life.
- 01:11:52 And, for us to do so, for us to start living a normal life again,
- 01:11:56 the vaccine is our only hope.
- 01:11:58 To get through this pandemic and future crises
- 01:12:01 we need stronger health systems to:
- 01:12:02 Improve effective vaccine delivery,
- 01:12:04 be better prepared for future health emergencies
- 01:12:06 support human capital development
- 01:12:09 [ANNUAL MEETINGS 2021 WASHINGTON DC]
- 01:12:11 [JULIETTE POWELL] Combating the pandemic
- 01:12:13 through the successful rollout of vaccination programs
- 01:12:16 requires collaboration across all levels.
- 01:12:19 The African Vaccine Acquisition Trust is a joint initiative between
- 01:12:24 the African Union,
- 01:12:25 he Africa Centers for Disease Control and Prevention
- 01:12:28 the World Bank and other African institutions.
- 01:12:31 And the whole idea is to fast-track
- 01:12:33 vaccine acquisition on the continent.
- 01:12:35 It's being heralded as an extraordinary regional effort
- 01:12:39 and I recently had the opportunity to speak
- 01:12:41 to Dr. Ahmed Ogwell, he's Deputy Director of the Africa CDC
- 01:12:46 about the importance of regional collaboration
- 01:12:49 and all of the challenges faced.
- 01:12:52 I'm joined now by Dr. Ogwell.
- 01:12:54 Let me begin by asking you this,
- 01:12:57 why is such a regional collaboration
- 01:12:59 so crucial in the fight of COVID-19,
- 01:13:02 but also to ensure better preparedness
- 01:13:04 for future health emergencies?
- 01:13:06 [DR AHMED OGWELL OUMA] Thank you for having me.
- 01:13:11 Collaboration within a region is very crucial,
- 01:13:14 and this is because
- 01:13:16 these countries and communities are neighbors,
- 01:13:19 they share the same, similar circumstances.
- 01:13:24 They share similar cultures and understanding.
- 01:13:28 Very often, they also share very similar capacities,
- 01:13:32 whether it is technical, knowledge or financial.
- 01:13:36 Leveraging on the expertise that is found within a region
- 01:13:40 is much easier than waiting for expertise
- 01:13:43 to come from far away.
- 01:13:44 Whether it is expertise in terms of knowledge
- 01:13:48 or whether it is equipment and infrastructure
- 01:13:52 in terms of laboratory and similar tools,
- 01:13:57 doing that within a region is so much easier.
- 01:14:01 Most of the regions today
- 01:14:03 are already geopolitically organized
- 01:14:06 into regional economic blocks or regional political blocks.
- 01:14:11 So working within a region like that
- 01:14:14 makes it much easier to gain consensus
- 01:14:17 and then be able to affect some action,
- 01:14:21 especially when it is required quickly.
- 01:14:24 Now, when you look at how do we prepare
- 01:14:28 for future possible health emergencies,
- 01:14:32 you find that regional response is better,
- 01:14:36 because you can quickly be able to share data,
- 01:14:38 you can quickly be able to share experts,
- 01:14:41 you can quickly be able to share resources
- 01:14:43 so that you respond in a very communal manner
- 01:14:47 in a group of countries,
- 01:14:49 and the effect is much faster in that way.
- 01:14:53 Therefore any health risk can be quickly brought under control.
- 01:14:59 [JULIETTE POWELL] The pandemic has highlighted
- 01:15:01 the risk of major disease outbreaks
- 01:15:03 and highlighted many countries'
- 01:15:05 lack of preparedness to fight them.
- 01:15:09 We've all seen the devastated human and economic fallout
- 01:15:13 and toll that this has taken.
- 01:15:15 But the Africa CDC is focusing
- 01:15:17 on disease surveillance, control and prevention,
- 01:15:21 as well as emergency preparedness.
- 01:15:24 Can you please tell us
- 01:15:26 what are the biggest challenges in this work
- 01:15:29 for you professionally and personally.
- 01:15:32 [DR AHMED OGWELL OUMA] Let me list a few.
- 01:15:34 One at the top of my list is supply chain.
- 01:15:38 One big challenge has been
- 01:15:40 how do we get the health products that we need
- 01:15:43 in preparedness and response
- 01:15:46 on to the continent and to ground zero,
- 01:15:50 where the health products are really required.
- 01:15:53 Whether it is as basic as masks,
- 01:15:55 or it is as complex as vaccines,
- 01:15:58 how do we secure that supply chain?
- 01:16:00 Africa is not manufacturing enough
- 01:16:02 of its own health products,
- 01:16:04 and this has been a huge challenge.
- 01:16:06 Something that we must address going into the future.
- 01:16:09 Second, is insufficient regulatory capacity
- 01:16:14 when you are bringing in health products of any type,
- 01:16:17 whether it's medicines, vaccines, diagnostics,
- 01:16:21 you want a regulatory system that works, and works quickly.
- 01:16:25 Now, Africa's regulatory system is not as strong,
- 01:16:28 and this is something that we need to build very quickly.
- 01:16:32 Third is workforce.
- 01:16:34 Where are those experts?
- 01:16:35 How many do you have?
- 01:16:37 How can you distribute them across the continent?
- 01:16:39 This has been a big challenge, because we don't have enough.
- 01:16:42 As widespread as nurses are,
- 01:16:47 they're not enough on the continent.
- 01:16:50 As few as epidemiologists,
- 01:16:51 the disease intelligence officers are,
- 01:16:53 they are very few on the continent
- 01:16:55 and everything in between.
- 01:16:56 So work force is a very critical challenge that we are facing.
- 01:17:00 Fourth are institutions.
- 01:17:02 Do you have institutions at country level
- 01:17:05 that can be able to guide preparedness and response?
- 01:17:08 Do you have institutions
- 01:17:09 at the continental level that are able to do that?
- 01:17:12 Well, luckily, at the continental level,
- 01:17:13 Africa cities there and we've been doing
- 01:17:15 a lot of this coordination,
- 01:17:17 but at country level, there are still gaps.
- 01:17:19 So I would say that these are
- 01:17:21 the four main challenges that we see
- 01:17:23 as far as preparedness and response is concerned.
- 01:17:27 An overarching challenge is the public.
- 01:17:31 How do you get the correct information to them?
- 01:17:34 And how do they respond to that correct information
- 01:17:37 in the middle of an avalanche of fake news
- 01:17:40 and half truths that are being pedaled in social media?
- 01:17:44 So this is a very overarching challenge,
- 01:17:47 in respect of what kind of outbreak
- 01:17:49 or health emergency we may be responding to.
- 01:17:52 Just prior to the COVID-19 pandemic,
- 01:17:55 the World Bank funded
- 01:17:57 the Africa CBC Regional Investment Financing Project.
- 01:18:00 The idea was to strengthen disease surveillance,
- 01:18:04 prevention and emergency response systems
- 01:18:06 across the African continent.
- 01:18:08 How is that kind of support,
- 01:18:10 from the World Bank and other institutions,
- 01:18:13 help the Africa CDC to grow over the past years,
- 01:18:16 and more to the point, what's next?
- 01:18:19 The World Bank has been a very good partner.
- 01:18:23 They came through for Africa CDC
- 01:18:27 at the beginning of the establishment of the agency
- 01:18:32 and supported us in three big ways.
- 01:18:36 One was to strengthen Africa CDC internally.
- 01:18:40 Our capacity, staffing.
- 01:18:44 This has been supported very effectively.
- 01:18:46 Second, is to strengthen
- 01:18:48 our ability to build our regional surveillance
- 01:18:53 and laboratory networks. We call that RISLNET.
- 01:18:56 This is where we bring together all the resources in a region,
- 01:19:00 so that they are working for a region
- 01:19:03 and not only for a country.
- 01:19:05 And that particulary, granted others,
- 01:19:07 has continued to help our work.
- 01:19:10 And third, is to build the capability
- 01:19:13 of Africa CDC to support our member States on the continent.
- 01:19:18 This is in many ways to build a capacity of the member States
- 01:19:23 and as well as to provide much needed infrastructure
- 01:19:27 for preparedeness and response.
- 01:19:29 Now, when we look into the future,
- 01:19:32 we are proposing that Africa CDC's new public health order
- 01:19:36 needs to be supported and implemented
- 01:19:39 so that we can effectively be able to prepare and respond
- 01:19:44 to health emergencies on the continent.
- 01:19:46 The new public health order has four plans.
- 01:19:50 One is strengthening institutions
- 01:19:52 for public health emergencies on the continent.
- 01:19:54 Both are the continental and national levels.
- 01:19:57 Second, is building the capacity of our workforce
- 01:20:01 that we require to respond to health emergencies.
- 01:20:05 Third, is local manufacturing of all the products that we need
- 01:20:10 from those are simple as masks
- 01:20:12 to those that are complex as vaccines.
- 01:20:14 We need to secure the supply chain on the continent.
- 01:20:17 And the fourth pillar is action oriented
- 01:20:20 and respectful partnerships
- 01:20:22 that are based on the priorities of Africa.
- 01:20:26 If we support the implementation of the new public health order,
- 01:20:30 Africa would be better prepared
- 01:20:31 for the next pandemic or the next outbreak.
- 01:20:34 [JULIETTE POWELL] Thank you so much, Dr. Ogwell.
- 01:20:36 It has been a joy to listen to you today.
- 01:20:39 It has been incredibly inspiring,
- 01:20:41 and we are very thankful for your time.
- 01:20:44 Thank you.
- 01:20:46 [WOMAN] Manao ahoana. I am [inaudible] from Madagascar
- 01:20:48 and you're watching the World Bank-IMF Annual Meetings.
- 01:20:54 [JULIETTE POWELL] How important to be reminded
- 01:20:56 that strong regional collaboration
- 01:20:58 and the sharing of data, expertise and resources
- 01:21:01 altogether can bring health emergencies
- 01:21:04 under control much more quickly.
- 01:21:06 Equitable access to vaccines is crucial
- 01:21:09 to ending the pandemic everywhere.
- 01:21:11 And we know that access
- 01:21:13 in developing countries remains very limited.
- 01:21:15 We've asked civil society leaders Priscilla Nyaaba,
- 01:21:20 executive director of Youth Harvest Foundation, Ghana,
- 01:21:23 and Nadia Daar.
- 01:21:24 She heads up the Washington D.C. office of Oxfam International
- 01:21:28 to share their thoughts and namely,
- 01:21:30 how limited access is affecting communities
- 01:21:33 and what their organizations are trying to do about it.
- 01:21:39 [PRISCILLA NYAABA] We have a mission
- 01:21:41 to support and empower young people
- 01:21:42 to achieve their full potential
- 01:21:44 in their personal life in their professional development,
- 01:21:47 for them to become active advocates
- 01:21:49 of the rights of young people.
- 01:21:51 Since the onset of COVID-19,
- 01:21:53 the Youth Harvest Foundation in Ghana collaborated
- 01:21:55 with Ghana Help Service
- 01:21:56 to create more awareness about the pandemic.
- 01:21:59 Using community radios,
- 01:22:00 information vans and on our social media platforms,
- 01:22:04 we created the Ghana COVID-19
- 01:22:06 Support Network platform on Facebook.
- 01:22:08 We also made donations of PPEs and other logistics
- 01:22:11 to the Ghana Help servicing the upper each region
- 01:22:14 to help fight the infection.
- 01:22:15 Some of the unforeseen effects
- 01:22:18 of low to no access to COVID-19 vaccines in Ghana
- 01:22:22 and in [inaudible]
- 01:22:24 is the limited access
- 01:22:26 to productive health services information
- 01:22:28 by women and girls, because of fear of being infected.
- 01:22:32 [NADIA DAAR] Low to no access to vaccines is resulting
- 01:22:35 in the world growing even more unequal.
- 01:22:38 Less than 1% of vaccines have gone to low-income countries.
- 01:22:42 26 people in Africa are dying every hour from COVID,
- 01:22:46 as they're told to wait for vaccine charity
- 01:22:48 from wealthy countries.
- 01:22:49 Donations are crucial,
- 01:22:51 but they're neither sustainable nor sufficient.
- 01:22:53 We have to address the monopoly control
- 01:22:56 that a few pharmaceutical corporations
- 01:22:58 have over vaccine price and supply.
- 01:23:01 Oxfam has been working with the People's Vaccine Alliance
- 01:23:04 to secure the temporary waiver
- 01:23:06 of intellectual property rules at the WTO.
- 01:23:08 While many are in favor,
- 01:23:10 we need all governments urgently agree
- 01:23:12 that the rights to produce these vaccines are shared,
- 01:23:15 to ensure the technology to produce them are transferred
- 01:23:18 via the WHO,
- 01:23:19 and that manufacturers around the world
- 01:23:21 have support to make them.
- 01:23:23 And we need the IFIs to use their extraordinary power
- 01:23:26 to help make this happen.
- 01:23:35 [JULIETTE POWELL] And that was a very good reminder
- 01:23:37 of the enormous disruptions in health care
- 01:23:39 that were caused by the pandemic,
- 01:23:41 and the impact that it's had on everyone,
- 01:23:44 even those not directly affected by the disease.
- 01:23:47 Find out more about how the Bank is responding to the pandemic
- 01:23:50 and accelerating vaccine delivery
- 01:23:52 at WorldBank.org/COVID-19.
- 01:23:57 And I'm joined once again by Sri.
- 01:24:00 I know that you've been following social,
- 01:24:02 so tell us what has stood up for you so far.
- 01:24:05 [SRI SRIDHAR] Thanks, Juliette.
- 01:24:06 So today's Hashtag was #vaccines4all,
- 01:24:09 and we've gotten a lot of comments
- 01:24:10 from folks all over the world,
- 01:24:12 including the United States, Venezuela,
- 01:24:15 Saudi Arabia, Spain, Ethiopia, India,
- 01:24:18 Ireland, the Switzerland, Uganda
- 01:24:20 and also the United Kingdom.
- 01:24:22 But what have people been talking about online?
- 01:24:25 Quite a few things.
- 01:24:26 They have been talking about the importance
- 01:24:28 of making vaccines more available to everyone,
- 01:24:31 as well as raising awareness about their safety,
- 01:24:34 about ensuring the technology to produce vaccines is shared
- 01:24:38 and also the importance of pandemic preparedness
- 01:24:41 and also disease surveillance.
- 01:24:43 We've also been monitoring some comments across social media,
- 01:24:46 so I did want to give a shout out
- 01:24:48 to a couple of comments that have come out on LinkedIn.
- 01:24:51 We have a comment here from Alex Mutiso,
- 01:24:53 who says that we now have a cure for malaria,
- 01:24:56 but let's work together to fight not just COVID,
- 01:24:59 but also other social, environmental and health issues
- 01:25:02 that impact the poor disproportionately.
- 01:25:05 So I think a good reminder
- 01:25:06 about some of the other major health crisis
- 01:25:09 still in the world today.
- 01:25:10 And we also have a comment from a Atul Save,
- 01:25:13 who says currently we are facing
- 01:25:15 a shortage of COVID-19 vaccines.
- 01:25:17 Many people are unable to get vaccinated
- 01:25:20 due to inadequate supplies,
- 01:25:21 which is something you and I
- 01:25:23 were just talking about a bit earlier
- 01:25:25 about that being quite a crisis.
- 01:25:28 Yeah, it's absolutely heart-breaking.
- 01:25:29 And I know that we have the poll.
- 01:25:31 Do we finally have those results?
- 01:25:32 Yes, we do have the poll results.
- 01:25:34 Today's poll asked what is most important
- 01:25:36 to ensure equitable and successful
- 01:25:39 COVID-19 vaccine deployment.
- 01:25:41 Now, as a reminder, the four choices were
- 01:25:44 was it having an adequate stock of vaccines,
- 01:25:46 a sufficiently funded, resilient and inclusive health system,
- 01:25:50 enough equipment and trained public health personnel,
- 01:25:53 or D, engagement of local community leaders
- 01:25:56 and organizations?
- 01:25:57 So before we get to the big reveal, how did you vote?
- 01:26:00 [JULIETTE POWELL] Alright, so if I had my druthers,
- 01:26:02 I would have said E all of the above.
- 01:26:05 [SRI SRIDHAR] Okay, that's a choice.
- 01:26:06 I went for A, but shall we see how people voted?
- 01:26:10 Okay.
- 01:26:14 So 44.3% of the votes goes
- 01:26:16 to a sufficiently funded resilient
- 01:26:18 and inclusive health system,
- 01:26:20 followed by having an adequate stock of vaccines,
- 01:26:23 enough equipment and trained public health personnel,
- 01:26:26 and finally engagement
- 01:26:27 of local community leaders and organizations.
- 01:26:30 [JULIETTE POWELL] Thank you so much, Sri.
- 01:26:31 [SRI SRIDHAR] Thanks, Juliette.
- 01:26:34 [MAN] Hi. I'm [inaudible], in Khartoum, Sudan.
- 01:26:36 And you're watching the World Bank-IMF Annual Meetings.
- 01:26:45 [MAN] ¡Hola! I'm [inaudible] in Montelíbano, Colombia,
- 01:26:49 and you're watching the World Bank-IMF Annual Meetings.
- 01:26:55 [JULIETTE POWELL] Our audience has been posting questions
- 01:26:58 before and throughout this entire broadcast,
- 01:27:01 and now we are joined live by two World Bank Group experts
- 01:27:05 to respond to some of those questions.
- 01:27:08 We have with us Mamta Murthi,
- 01:27:10 who is the World Bank vice president
- 01:27:12 for Human Development,
- 01:27:13 and Stephanie Von Friedeberg,
- 01:27:15 who is the senior vice president of Operations at the IFC,
- 01:27:18 which is the private sector arm of the Bank.
- 01:27:21 And thank you both for joining us today.
- 01:27:23 We really appreciate it.
- 01:27:24 We're going to start out by the most popular question
- 01:27:28 that came to us from our Francophone audience,
- 01:27:31 in particular.
- 01:27:32 And this is coming from Ndege Mamy Valerie.
- 01:27:36 She's in the Democratic Republic of Congo
- 01:27:39 and she sent us a video.
- 01:27:41 [HI, MY NAME IS NDEGE MAMY VALERIE]
- 01:27:44 [FROM THE DEMOCRATIC REPUBLIC OF CONGO]
- 01:27:47 [IN THE PROVINCE OF EQUATEUR.]
- 01:27:49 [MORE PRECISELY IN THE CITY OF MBANDAKA.]
- 01:27:51 [MY QUESTION IS: HOW HAS THE WORLD BANK ORGANIZED ITSELF]
- 01:27:55 [SO THAT THE DEVELOPING COUNTRIES CAN OBTAIN]
- 01:27:58 [AFFORDABLE ANTI-COVID VACCINES?]
- 01:28:01 [THANK YOU.]
- 01:28:05 [JULIETTE POWELL] I'd love to pose the question
- 01:28:06 to both of you, starting with you, Mamta.
- 01:28:08 And just to recap the question in English,
- 01:28:12 can you tell us just a little bit more about how you feel
- 01:28:16 the World Bank has organized itself
- 01:28:18 so that developing countries
- 01:28:20 can really obtain affordable COVID vaccines.
- 01:28:24 [MAMTA MURTHI] Thank you, Juliette, for that question.
- 01:28:26 And also thank you for the question coming in from DRC,
- 01:28:29 a country that I'm hoping to visit in a couple of weeks time.
- 01:28:33 I would say that the World Bank Group has done four things.
- 01:28:37 First of all, it's made a financing envelope available,
- 01:28:41 a significantly large financing envelope available
- 01:28:45 so that countries can buy these vaccines
- 01:28:48 and deploy them in country.
- 01:28:50 So as of a week or so ago,
- 01:28:53 already $6 billion had been committed
- 01:28:56 from this envelope to support purchase and deployment
- 01:29:01 in over 60 countries in the world.
- 01:29:05 From that money,
- 01:29:06 countries have already contracted nearly
- 01:29:09 a quarter of a billion doses of COVID-19 vaccines,
- 01:29:14 and a hundred million of those doses
- 01:29:16 will be delivered this calendar year.
- 01:29:19 So there's a part which relates to just resources for purchase.
- 01:29:24 The second part relates to support for deployment,
- 01:29:28 because as we've heard it's not enough
- 01:29:30 to get the vaccines to the country.
- 01:29:32 They actually have to go into people's arms.
- 01:29:35 And a lot of the support that we're providing
- 01:29:38 with partners on the ground is to support deployment.
- 01:29:42 You had this video from Côte d'Ivoire earlier, right?
- 01:29:46 Côte d'Ivoire is one of the countries
- 01:29:48 where the World Bank is working,
- 01:29:50 and we've supported the government
- 01:29:51 and ramping up vaccinations.
- 01:29:55 And we've done this by helping community leaders
- 01:29:59 and social influencers talk about vaccines
- 01:30:02 and how they're safe and how they're effective.
- 01:30:05 We're also supporting mobile clinics
- 01:30:07 that can go out to markets, to small villages,
- 01:30:09 tell people about the vaccines and also vaccinate them.
- 01:30:12 The third thing we're doing
- 01:30:14 is supporting the manufacturer of vaccines and peripherals.
- 01:30:19 And I have my colleague Stephanie here,
- 01:30:21 who's going to say a lot more about it.
- 01:30:23 So let me move on to the fourth thing that we're doing.
- 01:30:25 We're doing a lot of advocacy
- 01:30:28 so that developing countries
- 01:30:29 can have their vaccine contracts fulfilled.
- 01:30:32 And you heard from the Multilateral Leaders Task Force
- 01:30:36 from David, Kristalina, Tedros and others
- 01:30:39 about how important this is.
- 01:30:40 Because most of the vaccines have been delivered
- 01:30:43 and are being delivered in the richest countries of the world.
- 01:30:47 And we're saying
- 01:30:48 that manufacturers need to now reprioritize
- 01:30:51 and make sure that the contracts that are in place are satisfied.
- 01:30:56 The developing country contracts
- 01:30:58 that are in place need to be satisfied.
- 01:31:00 [JULIETTE POWELL] Absolutely.
- 01:31:01 I don't think anybody would disagree with that.
- 01:31:03 Stephanie, would you also like to respond to the question?
- 01:31:05 [STEPHANIE VON FRIEDEBURG] Absolutely, Juliette.
- 01:31:07 It's a great question.
- 01:31:08 It's a good follow on to the conversation
- 01:31:10 Mamta and I had at the Spring Meetings.
- 01:31:12 At the start of the Pandemic,
- 01:31:14 and you said this, IFC is the private sector arm
- 01:31:16 of the World Bank,
- 01:31:17 we actually thought our job was to ensure
- 01:31:20 that companies stayed afloat
- 01:31:21 and that we maintained jobs in our countries of operation.
- 01:31:25 So we created this $8 billion facility
- 01:31:27 for our existing clients and thought this is our way forward.
- 01:31:30 But then we quickly realized
- 01:31:32 that this wasn't just an economic crisis.
- 01:31:34 It was a health crisis, and we needed to do more.
- 01:31:37 And we could see from our conversations
- 01:31:40 with producers, and for people in our countries of operation,
- 01:31:44 that most of the equipment and the supplies,
- 01:31:46 to say nothing of vaccines,
- 01:31:47 were all being produced and consumed in the developed world.
- 01:31:51 And we knew we needed to do something different.
- 01:31:53 So we went back to our board, and we sought approval
- 01:31:57 for a $6 billion global health platform.
- 01:32:00 The idea was to help the production of PPE, equipment,
- 01:32:04 pharmaceuticals in our countries of operation.
- 01:32:07 And imagine when we did that,
- 01:32:09 we tacked vaccines on literally the last day
- 01:32:11 before we went to the board as a just in case.
- 01:32:14 So I'm actually really pleased to say that as of today,
- 01:32:17 we've invested $1.9 billion across the globe
- 01:32:21 in companies like Fosun in China,
- 01:32:24 Bio-E, who we heard from in India earlier today.
- 01:32:27 Our flagship project was a €600 million project
- 01:32:31 that we did with a group of DFIs
- 01:32:34 to produce 300 million doses of the Johnson & Johnson vaccine
- 01:32:39 on the continent of Africa
- 01:32:41 with a company called Aspen Pharmaceuticals.
- 01:32:43 But we know that that's not enough,
- 01:32:45 and we need to continue to push the envelope.
- 01:32:48 So we have created a new initiative with CEPI to help us.
- 01:32:52 We're partnering
- 01:32:53 with the Institut Pasteur in Dakar, Senegal,
- 01:32:56 to see if we can actually build an mRNA facility for later use.
- 01:33:00 And we're working very closely
- 01:33:02 with the government of Rwanda
- 01:33:04 to create an entire ecosystem to think through
- 01:33:07 how do you actually create
- 01:33:08 pharmaceuticals and vaccines on a more holistic basis?
- 01:33:12 It's a really heavy lift, but it's critical for us
- 01:33:15 as we move forward and come out of the crisis
- 01:33:18 to ensure that when the next pandemic hits,
- 01:33:20 our countries are better prepared.
- 01:33:22 [JULIETTE POWELL] I couldn't agree with you more.
- 01:33:24 And I'm glad to hear you talking
- 01:33:26 about assuring up the entire ecosystem.
- 01:33:28 I think that's absolutely fundamental.
- 01:33:30 We've got our second question for you,
- 01:33:33 and this is coming in
- 01:33:35 from [inaudible], he's in India.
- 01:33:38 And he asked:
- 01:33:40 can you predict the next era of COVID or pandemic?
- 01:33:46 [MAMTA MURTHI] That's a great question.
- 01:33:48 The answer to that is no one can predict
- 01:33:52 what the next pandemic will be or even when.
- 01:33:57 But what we can say with certainty
- 01:33:59 is there will be another pandemic.
- 01:34:01 Without a doubt.
- 01:34:02 We know, at least in the past 50 years or so
- 01:34:05 that most of these pandemics have arisen
- 01:34:08 because of the contact between humans and animals.
- 01:34:11 That's why they're called zoonotic.
- 01:34:14 And with urbanization, with intensive agriculture,
- 01:34:17 with what's happening globally,
- 01:34:19 we can expect another pandemic to emerge
- 01:34:22 because of this interaction between humans and animals.
- 01:34:27 We are saying that countries need to be prepared,
- 01:34:30 no matter when this arises, because it will arise.
- 01:34:34 And we really see four things as being important
- 01:34:38 for the next pandemic.
- 01:34:41 To fight it, countries need strong health systems.
- 01:34:44 We've learned from this pandemic
- 01:34:46 that if you don't have a strong core primary health care system,
- 01:34:49 you're not going to be able to detect
- 01:34:51 or treat or respond to the pandemic.
- 01:34:54 And so as the World Bank,
- 01:34:56 we're placing a lot of emphasis
- 01:34:57 on building strong health systems.
- 01:34:59 The second thing we've learned
- 01:35:01 is that you need regional and global cooperation.
- 01:35:05 I mean, a pandemic does not stop at the border.
- 01:35:08 It doesn't need a passport
- 01:35:09 to go from one part of the world to another.
- 01:35:11 And so we've also supported regional monitoring
- 01:35:15 and surveillance systems.
- 01:35:16 In Western Central Africa,
- 01:35:18 we have a great project which is called REDISSE,
- 01:35:21 and it's actually supported networked surveillance
- 01:35:24 and monitoring systems
- 01:35:26 to detect and respond to emerging diseases.
- 01:35:29 We've also supported the Africa Center for Disease Control,
- 01:35:33 which has been playing a fantastic role in this pandemic.
- 01:35:37 It's not just regional cooperation.
- 01:35:39 One needs to think of multisector responses.
- 01:35:42 Think of this pandemic.
- 01:35:43 One of the ways of responding to it
- 01:35:46 was asking people to stay at home
- 01:35:48 so that it would not spread.
- 01:35:50 But if you ask people to stay at home,
- 01:35:51 how are they going to earn an income?
- 01:35:53 And that's why having some sort
- 01:35:55 of cash benefit or transfer was very important.
- 01:35:58 Both for households, but also for small businesses.
- 01:36:02 A multi sector and a multicountry response
- 01:36:05 is the second thing we've learned is necessary.
- 01:36:08 The third thing we've learned is distributed manufacturing.
- 01:36:12 That's the key to having some kind of global health security.
- 01:36:15 And I think IFC and others
- 01:36:17 play an incredibly important role here.
- 01:36:19 And I think the final thing that we've learned
- 01:36:22 is that you really need to fund these things adequately.
- 01:36:26 We heard Ngozi talk this morning earlier today
- 01:36:29 about how countries need to spend much more themselves.
- 01:36:32 Right.
- 01:36:33 She talked about a 1% increase in GDP spending
- 01:36:37 to support pandemic preparedness.
- 01:36:40 And she also talked about better network global architecture.
- 01:36:44 So we need all of these things
- 01:36:46 so that we can prepare for the next pandemic,
- 01:36:49 even though we don't know exactly what it's going to be.
- 01:36:53 [JULIETTE POWELL] I feel like you've, in part,
- 01:36:54 answered our final question today.
- 01:36:57 This was the most popular question
- 01:36:59 that was sent in by the audience that's watching.
- 01:37:02 They really want to know the answer to this question,
- 01:37:06 which is what kind of transformation is needed
- 01:37:09 for health care systems in poor countries?
- 01:37:11 In other words,
- 01:37:12 how do we make the health systems more resilient
- 01:37:16 now and in the future?
- 01:37:19 How does that work?
- 01:37:21 [MAMTA MURTHI] I would say they have to be stronger.
- 01:37:24 They have to be better resourced with trained personnel
- 01:37:29 with the ability to surge, right?
- 01:37:32 Suppose you have the emergence of a disease,
- 01:37:34 you need more people working on it.
- 01:37:36 You need the ability to detect and prevent disease.
- 01:37:42 And that means you really have to take a one health approach.
- 01:37:45 You've got to look not just at human disease,
- 01:37:48 but you've got to look at animal disease
- 01:37:50 and how these two are interacting.
- 01:37:53 And then I think you need
- 01:37:54 strong regional and global institutions.
- 01:37:57 I like very much what Kristalina said
- 01:38:00 at the end of the leader segment
- 01:38:02 where she said, what this pandemic has done is
- 01:38:05 it's shown that if you have a weak immune system,
- 01:38:08 you're going to fall sick.
- 01:38:10 It's the same with countries.
- 01:38:11 If you don't have a resilient health system
- 01:38:14 or a means of dealing with an emergency,
- 01:38:16 you're not going to be able to deal with a pandemic.
- 01:38:19 So I think institutional development,
- 01:38:21 starting with strong health systems,
- 01:38:23 is probably what's needed.
- 01:38:24 [JULIETTE POWELL] Stephanie, did you have a thought
- 01:38:26 really briefly before we go on?
- 01:38:28 [STEPHANIE VON FRIEDEBURG] So I actually do.
- 01:38:31 When I look at the conversation we've had,
- 01:38:34 we've been talking a lot about shots and arms,
- 01:38:36 which was a critical imperative for us in the short term.
- 01:38:40 But we need to redouble our efforts
- 01:38:42 to build a more holistic system around the world
- 01:38:45 and at the country level.
- 01:38:47 And that really starts with thinking
- 01:38:49 about things like how do we get modern equipment
- 01:38:52 into places like Africa?
- 01:38:54 So one of the things that we've been working on
- 01:38:57 is a $300 million African medical equipment facility.
- 01:39:00 What it's designed to do...
- 01:39:02 We've partnered with GE and Philips and others,
- 01:39:05 and we're giving equipment through leases
- 01:39:08 and through acquisition to small clinics in Africa,
- 01:39:11 using financial institutions as intermediaries.
- 01:39:15 And why are we doing this?
- 01:39:16 So if you look at Africa,
- 01:39:18 WHO did a recent study that said
- 01:39:20 that only 11% of the countries in Africa
- 01:39:24 have one MRI machine for 1 million people,
- 01:39:28 and 24% for CT scans.
- 01:39:30 If you compare that to Europe,
- 01:39:33 countries in Europe have 89% better statistics on MRI
- 01:39:39 and 97% better statistics on CT scanners.
- 01:39:43 So we know we need to solve the fragmentation in Africa.
- 01:39:47 And working with GE and Phillips,
- 01:39:49 we can do that and bring the right technical skills.
- 01:39:51 I think the other thing that Mamta didn't mention,
- 01:39:54 which we've seen very repeatedly
- 01:39:56 is the need for public-private partnership.
- 01:39:59 So we've learned in our other countries of operation
- 01:40:01 that you can do this through public-private partnerships.
- 01:40:05 We've done really interesting work
- 01:40:06 in Turkey with hospitals,
- 01:40:08 and in Uzbekistan recently with dialysis clinics.
- 01:40:11 The other thing is we really need
- 01:40:13 to double down and focus on education.
- 01:40:15 And I think this is an area
- 01:40:17 where the Bank and IFC can really work together.
- 01:40:19 We need health technicians,
- 01:40:21 we need nurses and we need doctors at scale
- 01:40:23 to really make this work.
- 01:40:25 [JULIETTE POWELL] I couldn't agree with you more.
- 01:40:27 Thank you both for joining us,
- 01:40:29 and thank you for working together.
- 01:40:32 and to you, our viewers,
- 01:40:34 please do continue to post those questions.
- 01:40:36 We've got experts here
- 01:40:37 that are going to stay online
- 01:40:38 and they're really going to do their best
- 01:40:41 to answer all of them for you.
- 01:40:43 Young people have been deeply impacted by this pandemic
- 01:40:47 with the closing of schools.
- 01:40:49 You've got separation from friends and from family.
- 01:40:51 They're all struggling to cope,
- 01:40:53 and they worry about being left behind, and with good reason.
- 01:40:56 But they're also incredibly optimistic about their futures.
- 01:41:00 So we asked some young people from around the world
- 01:41:03 to talk about what it was
- 01:41:04 that the vaccine means for them and their communities,
- 01:41:08 and what they can really look forward to doing
- 01:41:10 once they're vaccinated.
- 01:41:15 [RADHIKA BATRA] COVID has devastated us all
- 01:41:17 due to loss of lives,
- 01:41:18 financial loss, loss of jobs.
- 01:41:21 [COVID-19 HAS BROUGHT A NEGATIVE IMPACT ON MY LIFE OVERALL.]
- 01:41:24 [IT'S DEFINITELY SOMETHING THAT I, AN ALL OF US,]
- 01:41:28 [DID NOT EXPECT.]
- 01:41:29 [SEDIGHE KARIMZADEH] Currently we lack basic sanitation
- 01:41:32 and health services.
- 01:41:33 We are at greatest risk of transmission.
- 01:41:36 [FANNY BESSEM] Because many of the results
- 01:41:38 that we are available have been diverted to COVID.
- 01:41:42 It's very challenging,
- 01:41:44 and the mental health issues are just tremendous.
- 01:41:47 [LAVAU NALU] I haven't seen a lot of my family
- 01:41:49 and a lot of my friends for so long
- 01:41:51 and I can't wait for that day when we're all here together.
- 01:41:54 [MIRIAM LIVRAMENTO] I believe in science,
- 01:41:55 I believe in immunization
- 01:41:57 through vaccination.
- 01:41:58 [YANA PANFILOVA] On behalf young people,
- 01:42:00 the most important thing:
- 01:42:01 the vaccine gives us assurance that we will not be locked down.
- 01:42:07 We will not again feel the weight of this pandemic
- 01:42:11 on our shoulders.
- 01:42:13 [PATELISIO PATELISIO] Getting vaccinated means
- 01:42:14 I get to protect myself
- 01:42:16 and my family.
- 01:42:17 [MIRIAM LIVRAMENTO] It means we can have these streets
- 01:42:20 full of turists again.
- 01:42:22 And we can have opportunities for young people like me
- 01:42:25 to grow our business.
- 01:42:27 [MAMELLO MAKHELE] Once I get vaccinated against COVID-19,
- 01:42:30 I'll be able to socially interact with my friends
- 01:42:33 without fear of being sick.
- 01:42:35 [LAVAU NALU] Being vaccinated means
- 01:42:37 that my family can be reconnected here,
- 01:42:39 in Papua New Guinea [inaudible].
- 01:42:41 [RADHIKA BATRA] We will live without the fear
- 01:42:42 of losing a loved one.
- 01:42:43 There will be jobs and food on the table.
- 01:42:46 [EMMANUELE MARIE PARRA] I can attend and hear
- 01:42:48 live masses in Church with family.
- 01:42:50 [FANNY BESSEM] Our lives can go back to normal.
- 01:42:52 We can go to markets.
- 01:42:53 We can attend our family meetings.
- 01:42:55 We can go to the communities and work without fear.
- 01:42:58 [CARLOS MADRIGAL IBERRI] We can go back to the streets
- 01:43:00 with the patients,
- 01:43:02 so we can get to transform the hearts
- 01:43:04 of the population in Mexico.
- 01:43:06 [SEDIGHE KARIMZADEH] So getting vaccinated would mean
- 01:43:09 we can still take one more step to save our lives.
- 01:43:12 -[PATELISIO PATELISIO] We want... -[MAMELLO MAKHELE] ...to get vaccinated...
- 01:43:14 - [YANA PANFILOVA] ...so life... - [SEDIGHE KARIMZADEH] ...can return
- 01:43:15 [CARLOS MADRIGAL IBERRI] ...to normal.
- 01:43:22 And this brings us to the end of this event.
- 01:43:25 I really want to thank our guests for joining us
- 01:43:27 and sharing an incredibly important discussion.
- 01:43:30 Of course, I want to thank you, our viewers.
- 01:43:32 We've still got much more to come
- 01:43:34 for these Annual Meetings on Thursday.
- 01:43:36 We're going to be discussing
- 01:43:38 how we can make climate action count
- 01:43:40 and then to round off the week,
- 01:43:42 we're going to be focusing
- 01:43:43 on the role of trade in supporting economic growth.
- 01:43:46 Of course, you can watch all of those
- 01:43:48 as well as replay of this event at live.WorldBank.org.
- 01:43:52 And of course,
- 01:43:53 we hope that you've all enjoyed hearing
- 01:43:55 from our distinguished guests at today's event.
- 01:43:58 And do continue sharing all of those comments,
- 01:44:01 we'd absolutely love to hear from you again.
- 01:44:03 My name is Juliette Powell,
- 01:44:04 and thank you so much for joining us today!

ANNUAL MEETINGS 2021
Tune in, ask questions, and share your views with participants from all over the world during the 2021 Annual Meetings of the World Bank Group and the International Monetary Fund (IMF).
Watch the World Bank Group public events:
Oct. 11: Growth in a Time of Crisis
Oct. 12: Civil Society Townhall
Oct. 12: Ending the Pandemic
Oct. 13: Opening Press Conference
Oct. 14: Making Climate Action Count
Oct. 15: Trade to the Rescue